Welcome to the Leeds Centre for Women’s Health. You have received this leaflet because you have been diagnosed with an Ectopic pregnancy. This leaflet will explain what it is and how it is treated.
What is an ectopic pregnancy?
An ectopic pregnancy is a pregnancy that develops outside the uterus (womb). Around 1 in 90 pregnancies in the UK is an ectopic pregnancy.
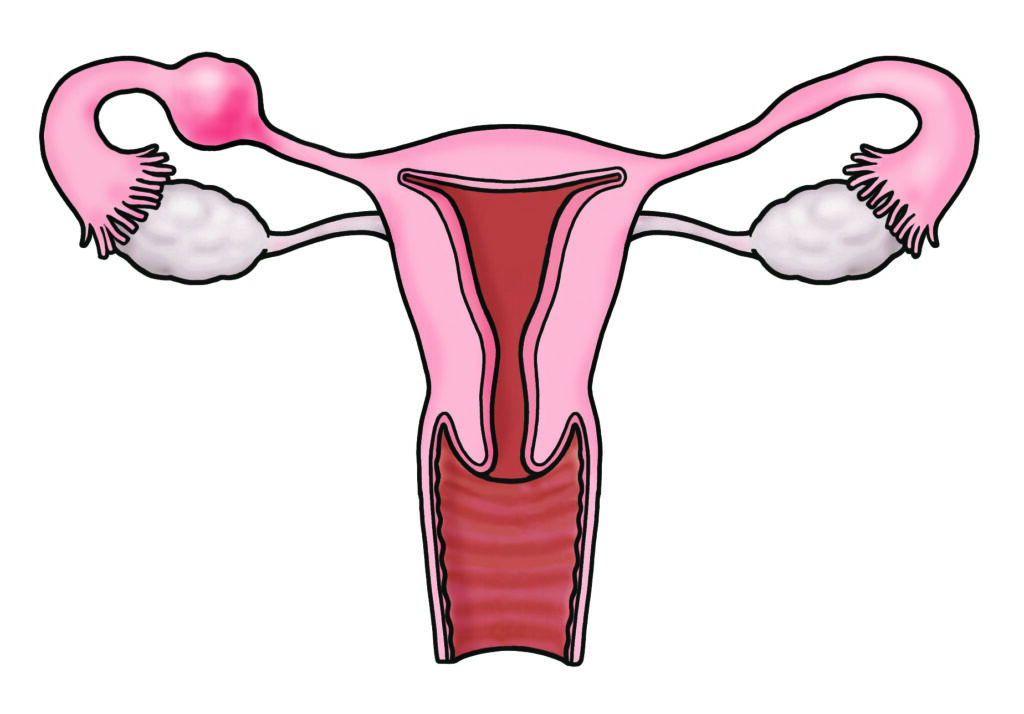
Normally when you become pregnant, the sperm fertilises the egg in one of your two fallopian tubes (the tubes that carry the egg to the womb).The fertilised egg then moves into the uterus, implants and grows. In an ectopic pregnancy this process does not happen and the pregnancy implants elsewhere.

An illustration of the sperm swimming through the cervix, womb and fallopian tube to reach the egg released by the ovary, and the egg moving into the womb.
Most ectopic pregnancies occur in the fallopian tube (95%) but they can rarely be found elsewhere including on the ovary, abdomen, cervix (neck of the womb) and scar of a previous Caesarean section.
An illustration that shows a swelling in the tube where the pregnancy has got stuck.
Why does an ectopic pregnancy happen?
Risk factors for an ectopic pregnancy include:
- Having had an ectopic pregnancy in the past.
- Having damaged fallopian tubes. Causes of damaged tubes include:
– Previous pelvic infection.
– Previous surgery to fallopian tubes including sterilisation.
– Previous abdominal or pelvic surgery including appendicitis.
- Getting pregnant with the intrauterine device (IUD/coil) or when on the progesterone only pill (minipill).
- Having conceived by assisted reproduction such as IVF.
- Being over 40 years old when you get pregnant.
- Smoking.
What are the symptoms of an ectopic pregnancy?
Sometimes you might not have any symptoms and are only diagnosed when you have an ultrasound scan.
Symptoms of an ectopic pregnancy may be vague and can make the diagnosis difficult to make. These symptoms usually occur between the 4th and 10th week of pregnancy and include:
- Pain in the lower part of the abdomen – usually more on one side and normally progressively getting worse.
- Pain at the tip of the shoulder(s).
- Irregular vaginal bleeding- may be light or a brown vaginal discharge.
- A missed or late period.
- Bowel problems- diarrhoea as well as pain when going to the toilet.
- Feeling light-headed or fainting.
- No symptoms at all.
How is an ectopic pregnancy diagnosed?
An ectopic pregnancy can be difficult to diagnose. One of the first things you will be asked for is a urine sample for a pregnancy test.
A negative test means that it is very unlikely that your symptoms are due to an ectopic pregnancy.
Usually a diagnosis of ectopic pregnancy is made using a combination of the following:
A medical review and external and internal examinations
Your medical history and the background to this episode are important. Your pulse, blood pressure and temperature will be taken. The doctor or nurse will ask your permission to examine your tummy and internally. A female will be present to support you.
Pelvic ultrasound scan
You may be offered a transvaginal ultrasound scan (where a probe is inserted into the vagina) to look at your uterus, ovaries and tubes. Sometimes you are asked to return for a repeat scan if a pregnancy cannot be seen on the first scan.
Human chorionic gonadotrophin (hCG) blood test
This is the pregnancy hormone which is measured positive or negative in urine. In the blood, the amount can be measured precisely. The amount changes every day and this is a useful tool to help reach the right diagnosis when it is not yet clear where the pregnancy is located or whether it may be a simple miscarriage or a more dangerous ectopic pregnancy.
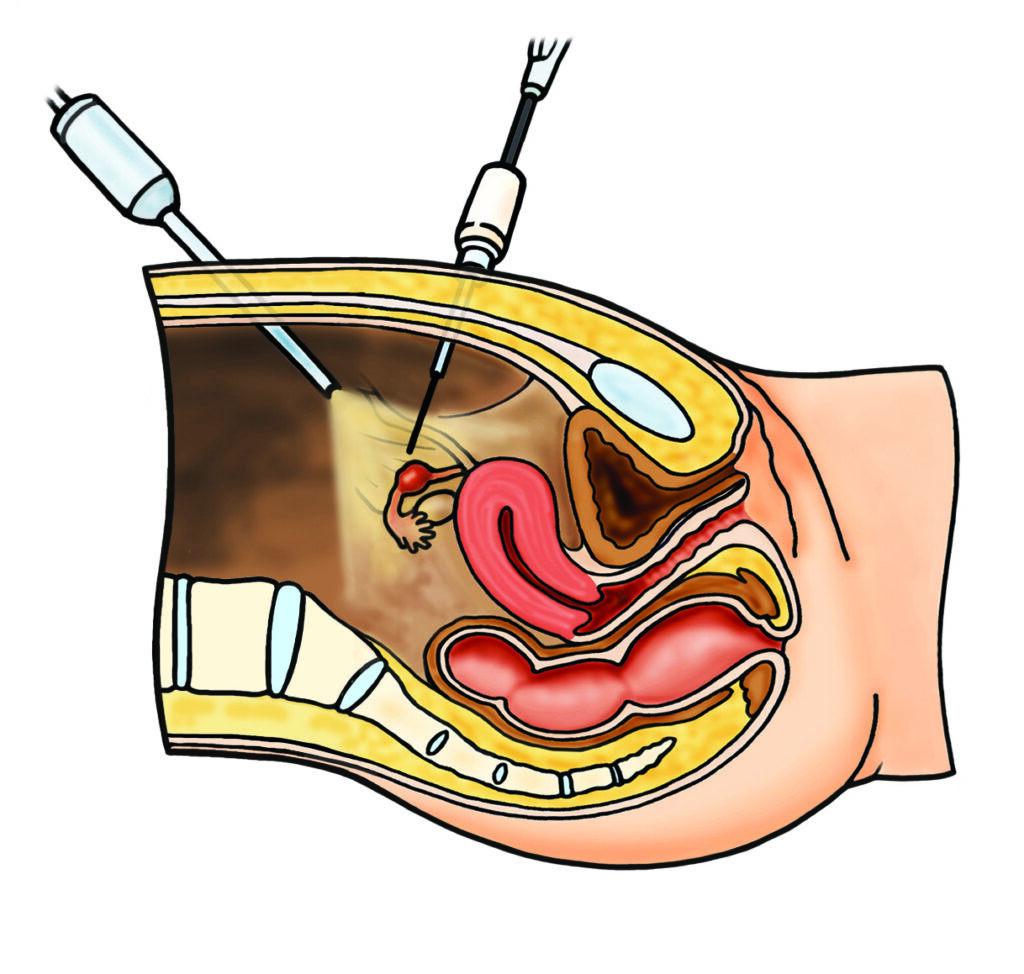
Laparoscopy
A laparoscopy is a key-hole operation done under general anaesthetic (where you are put to sleep). A telescope is inserted into the belly button through a small cut to look at the womb, tubes and ovaries from the inside. If an ectopic pregnancy is found, it will be removed at the same time, usually with keyhole surgery techniques. Please see separate patient information on laparoscopy if this is recommended to you.
How is an ectopic pregnancy treated?
There are different ways to treat an ectopic pregnancy. Not all options will be suitable for you. Your doctor will discuss the ones that are.
- Expectant management (wait, see and monitor).
- Medical management.
- Surgical management.
The options you are offered will depend on:
- The severity of your symptoms.
- If there is bleeding inside your abdomen.
- The level of your pregnancy hormone (hCG level).
- Your scan result.
- Your general health.
- Your views and preference.
Expectant Management
This can be offered to you if:
- You are clinically stable and pain free.
- You have a pregnancy thought to be in your fallopian tube which is small and there is no fetal heart beat.
- You HCG (pregnancy hormone) level is low, 1000 iu/L or less, or if they are between 1500 and 1000/iu/L and falling.
- You are able to return to the hospital for follow up.
If you are being offered expectant management we would perform the HCG levels on days 2, 4 and 7 after your diagnosis.
If the levels are dropping you will be asked to attend for weekly HCG levels until a negative result (less than 20 IU/L).
If the HCG levels are not falling (for example if they stay about the same or rise) we would check how you are doing and consider offering you further management. There is a small chance you may require emergency surgery if you develop severe pain and there is evidence of a ruptured ectopic pregnancy.
Provided you meet the criteria for being offered expectant management (listed above) there appears to be no difference in outcome between expectant or medical management in the rate of ectopic pregnancies ending naturally, the risk of rupture, the need for additional treatment or your health status.
It is also likely that the time taken for the ectopic pregnancy to resolve and your future fertility outcomes are the same with either expectant or medical management.
Medical Management
Ectopic pregnancies can sometimes be treated with medication. The fallopian tube is not removed.
The medication (methotrexate) prevents the pregnancy from developing and the ectopic pregnancy gradually disappears. Methotrexate is given as an injection into a muscle in your body e.g. bottom.
Methotrexate is not suitable if:
- You are unwell and the doctors are concerned that you are bleeding internally.
- You have a lot of pain in your abdomen.
- Your pregnancy hormone levels are very high.
- You have medical issues that mean you should not have methotrexate.
The advantages of methotrexate are:
- It works 70 – 80% of the time.
- You avoid having an operation with all its risks.
- You usually do not need to stay in hospital more than a night, if at all.
The disadvantages of methotrexate are:
- It may not work, or may not work well-enough first time.
- You may need a further dose of methotrexate if your pregnancy hormone levels aren’t falling (15% of cases).
- You may need surgery (less than 7% of cases) if you become unwell.
- You may experience side-effects from the treatment: abdominal pain (common but brief), nausea (common but brief), mouth ulcers and skin rashes (uncommon).
- You will be advised to wait for three months after the injection before trying for another pregnancy to make sure the medication is out of your system.
- You will need to return for a blood test (hCG levels) twice in the first week and then until they return to pre-pregnancy levels. This takes an average of 6 weeks.
Surgical Management
Surgical management of ectopic pregnancy is done under general anaesthetic (asleep).
This may be recommended treatment if:
- You are unwell.
- There is a live ectopic pregnancy.
- Your hormone level is very high.
- The diagnosis remains uncertain.
The procedure is either performed by:
- Laparoscopy (key-hole surgery).
- Laparotomy (open surgery usually through a bikini line cut in the lower part of the stomach).
Usually the procedure is done by key-hole surgery. This involves making three or four small cuts to the abdomen so that a camera can be inserted and the pelvis can be directly viewed. Instruments can then be used to remove the ectopic pregnancy.
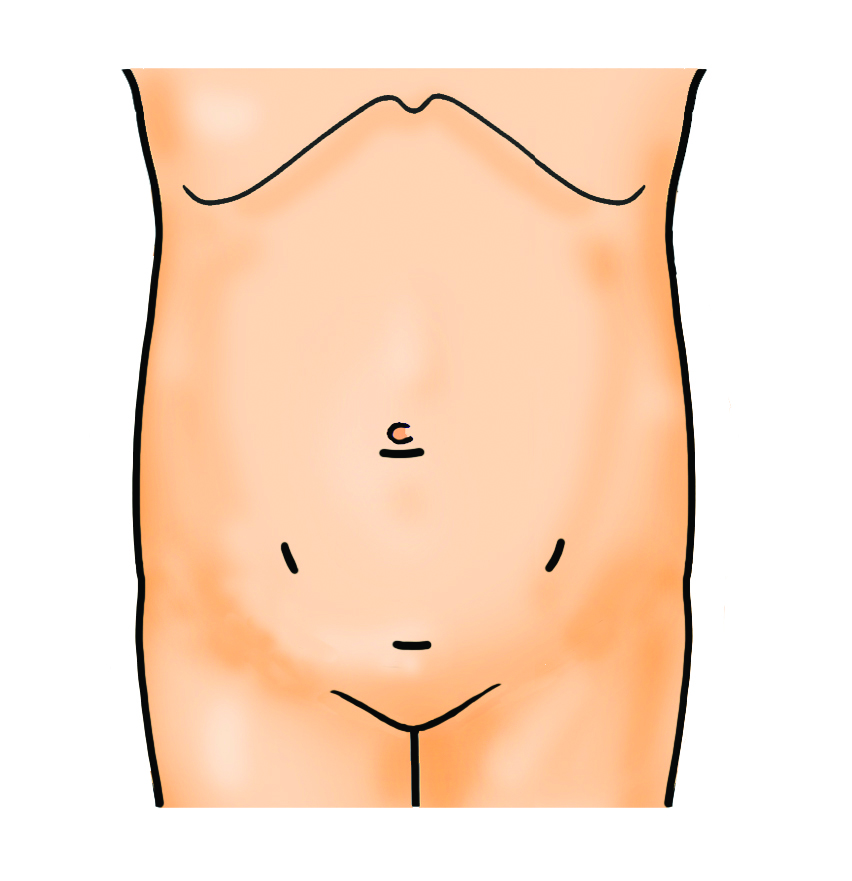
An illustration that shows the likely position of gynaecology keyhole surgery scars (3-4 below the belly button, 5-10mm in size broadly in a circle formation).
Laparoscopic surgery shortens the length of time you need to stay in hospital and your recovery when you get home compared to an open operation. Physical recovery is usually two weeks.
Please see
Separate information on diagnostic laparoscopy for more detail on the risks.
A laparotomy (open surgery) is done if:
- You are too unwell.
- You have had previous abdominal surgery.
- There are technical difficulties with the operation that mean the doctors are unable to complete the procedure by key-hole route.
Please note
Physical recovery is usually six weeks for open surgery.
Salpingectomy
If an ectopic pregnancy is seen then normally the affected tube is removed completely with the pregnancy tissue inside.
Salpingostomy
Occasionally the ectopic pregnancy is removed from the tube and the tube is left. This may be considered for you if you have already had a tube removed previously.
This gives you a chance to get pregnant naturally in the future.
The disadvantages of salpingostomy are:
- It increases the chance that not all the ectopic pregnancy has been removed (up to 25% of cases). You will need to be monitored after the operation with pregnancy hormone blood tests to make sure that your levels are falling.
- There is an increased risk that you will need to go back to the operating theatre for a second operation to remove the tube if it continues to bleed.
- There is a higher risk of another ectopic pregnancy in the future.
If your tube has been removed you will be advised to do a pregnancy test three weeks after surgery. If the ectopic pregnancy has been removed but the tube has been left behind then you will need to have regular pregnancy blood tests until the level has fallen to normal (negative).
Disposal of pregnancy tissue
When you have an operation for a pregnancy complication you will be asked to sign a form giving instructions (consent) to the hospital about how you would like the tissue that is removed to be handled and disposed of. The doctor will explain your options. This may be done before or after the surgery, depending on how unwell you are.
Anti-D
Anti-D is an antibody injection given if your blood group is Rhesus-D negative to prevent you from producing antibodies to the current pregnancy which could cause problems to the baby in a future pregnancy. Your doctor can explain more if necessary.
When to expect your next period
After an ectopic pregnancy
Has been removed or treated you will need to do a urine pregnancy test after three weeks, If it is POSITIVE, please contact GATU by telephone for further instructions.
It is likely that you will get a period about 6 – 8 weeks after completing treatment but it may take up to six months. Please seek advice from your GP if you have any concerns.
You may not get a period if you have had the contraceptive implant or injection.
When is it safe to start having sex again?
Medically, it is safe to have sex once any vaginal bleeding and discharge have stopped. However, if you are feeling tired and/or you are still sore or in pain you may want to wait longer. Emotionally, you may want to wait longer.
Emotional recovery
Everyone copes differently following an ectopic pregnancy.
You may feel some of the following:
- Upset or fear over the experience.
- Worry about getting pregnant again.
- Grief or shock.
- Guilt or blame over what has happened.
Please feel free to talk about these concerns with the gynaecology doctors and nurses on Ward J24, Gynaecology Acute Treatment Unit and the Early Pregnancy Unit.
How does this affect any future pregnancies?
The chance of having an ectopic pregnancy in the future is 7 – 10%. However the chance of a successful pregnancy in the future is good. Removal of a fallopian tube only slightly reduces your chance of falling pregnant particularly if the remaining tube is normal.
You will be advised to have an ultrasound scan at 6 to 8 weeks during your next pregnancy to confirm that the pregnancy is developing in your womb.
What contraceptives can I use?
You can become pregnant as early as ten days following the end of your pregnancy. If you do not want to become pregnant you can seek advice on forms of contraception from your GP.
At the Gynaecology Acute Treatment Unit (GATU, Ward J24A), we may be able to offer the hormonal contraceptive implant and injection. Ask the doctor or nurse caring for you for more details.
Informed Consent
This leaflet is provided to supplement verbal information that will be given to you by your healthcare provider (Doctor/ Surgeon/ Nurse) as part of the consent process prior to your procedure. Information sharing between you and the clinician is essential to ensure that your decision to consent is fully informed.
Please ask questions if you don’t fully understand or have any concerns about what is proposed. You have a right to be involved in these decisions and should feel supported to do so. Please take the time to consider what is important to you to ensure the information you receive is specific and individualised.