This leaflet gives information to help you prepare for your anaesthetic. It has been written by anaesthetists working together with patients and patient representatives. It also shows you where to find other information that might be helpful.
What is anaesthesia?
Anaesthesia stops you feeling pain and unpleasant sensations. It can be given in various ways and does not always need to make you unconscious. There are different types of anaesthesia, depending on the way they are given:
Local anaesthesia:
Involves injections that numb a small part of your body. You stay conscious but free from pain.
Regional anaesthesia:
For example a spinal or epidural, involves injections that numb a larger or deeper part of the body. You stay conscious or receive some sedation, but are free from pain. For some surgery you may be aware of pressure sensations.
General anaesthesia:
Gives a state of controlled unconsciousness. It is essential for some operations and procedures. You are unconscious and feel nothing.
Sedation:
Gives a ‘sleep like’ state and is often used with a local or regional anaesthetic. Sedation may be light or deep and you may remember everything, something or nothing after sedation.
Anaesthetists
Anaesthetists are doctors with specialist training who:
- Discuss with you the type or types of anaesthetic that are suitable for your operation. If there are choices available, they will help you choose.
- Discuss the risks of anaesthesia with you.
- Agree a plan with you for your anaesthetic and pain control afterwards.
- Give your anaesthetic and are responsible for your wellbeing and safety throughout your surgery and in the recovery room.
You may also meet Anaesthesia Associates who are highly trained healthcare professionals.
The Pre-assessment Patient Guidance
This outlines the process for preparing for a planned operation, ensuring patients are ready for surgery and anaesthesia. Here’s is a summary:
E-Care Self-Assessment
You’ll receive a text with an e-care self-assessment form. Complete it promptly and accurately. If you have trouble, contact the team at 0113 206 5769 or 0113 206 5685. After submission, the nursing team may call to discuss your procedure, and you’ll be invited for clinical tests.
In-Person Assessment
Some patients may need to visit the department for a discussion with a nurse or anaesthetist.
Pre-Assessment Team’s Role
- Review your medical history to determine the type of
- pre-assessment needed.
- Identify necessary clinical tests.
- Provide advice on preparing for anaesthesia (refer to “Shape Up for Surgery” guidance).
- Remind you to have post-operative pain relief ready at home.
- Supply surgery-specific information leaflets during your clinic visit.
Information Collected
- Past medical history.
- Allergies, reactions, or issues with previous anaesthetics.
- Current medications.
- Lifestyle factors (e.g., smoking, alcohol, recreational drug use).
Possible Clinical Tests
- Blood tests.
- ECG (heart tracing).
- Infection prevention checks/swabs.
- Height and weight measurement.
- Blood pressure, heart rate, and oxygen level checks.
- Urine test.
This process ensures you’re medically prepared for surgery and helps tailor care to your needs. For further details or assistance, contact the provided numbers.
Before coming to hospital
There is much you can do to prepare yourself for surgery and the recovery period.
- If you smoke, giving up several weeks before the operation will reduce the risk of breathing problems during your anaesthetic and after your surgery.
- If you are obese, reducing your weight will reduce many of the extra risks you face during your anaesthetic and after your surgery. It may also make the surgery easier.
- If you have loose teeth or crowns, a visit to your dentist before the operation may reduce the risk of damage to your teeth during the anaesthetic.
- If you have a long-standing medical problem that you feel is not well controlled (eg diabetes, asthma or bronchitis, thyroid problems, chronic pain or heart problems), check with your GP surgery whether there is anything you can do to improve it.
- It is also important that you consider any mental health concerns such as anxiety and depression, as these too can make a difference to your surgery and recovery.
- Increasing your activity in the weeks before surgery can improve your heart function and fitness levels. Studies have shown that this can make a big difference to your recovery from surgery.
- It is best to plan early for your recovery at home afterwards and let your friends and family know how they can best help you. Think about what you will eat and whether you need to make any changes at home to make your recovery easier.
- If you return home the same day having had a general anaesthetic or sedation, you will need to organise a responsible adult to take you home by car or taxi and stay with you for up to 24 hours.
- It is important to think how you can best relax on the day of your operation as you may have to wait before your surgery. Magazines, puzzles or listening to music through headphones can all be helpful.
- Please note that family visitors are not permitted in admission, theatre and recovery areas (only allowed in special circumstances).
On the day of your operation
The hospital should give you clear instructions about eating and drinking. These instructions are important. If there is food or liquid in your stomach during your anaesthetic, it could come up into your throat and lungs and endanger your life.
Diabetes:
Please check with your hospital about when to stop eating and drinking and how you should take your medication on the day of your operation.
Smoking:
You should not smoke on the day of your operation, as this reduces the amount of oxygen in your blood. You should also not vape.
Medication:
You should follow the specific instructions from the preoperative assessment team about how to take them on the day of the operation. You will be allowed a sip of water to take any tablets as needed.
If you take any ‘blood thinning’ drugs such as warfarin, clopidogrel or rivaroxaban, you will need to discuss with your consultant or the preoperative assessment team whether or when you should stop taking them.
They will look at any risks of bleeding and risks of stopping the treatment and make a plan with you. Your nurse will give you clear instructions before your surgery.
Feel unwell:
When you are due to come into hospital, please telephone the ward for advice.
Please remove nail varnish or gels before coming to the hospital. This ensures that the clip on your finger to measure oxygen levels works well during your anaesthetic.
Meeting your anaesthetist
Your anaesthetist will meet you before the operation. This may be in the preoperative assessment clinic or on the day of your operation. They will discuss the type of anaesthetic you might have, including benefits, risks and your preferences.
On some occasions, you will be seen by an Anaesthesia Associate, who is a trained, skilled practitioner that works within the anaesthetic team under the supervision of a Consultant Anaesthetist. They will decide with you which anaesthetic would be best for you. Not all types of anaesthesia are appropriate for all types of operations.
If there is a choice of anaesthetic, the decision on which to use will depend on:
- The operation you are having and any medical problems.
- Your particular risks.
- Your preferences and the reasons for them.
- The recommendation and particular skills of the anaesthetist.
- The equipment, staff and resources at the hospital.
Questions you may like to ask your anaesthetist or nurse
If you have questions about your anaesthetic, write them down or consider the examples opposite. If you want to speak to an anaesthetist before the day of your operation, contact the preoperative assessment team who may be able to arrange for you to speak to an anaesthetist on the phone or to see them in a clinic.
Getting ready for your operation
Your nurse will give you a hospital gown to wear and discuss what underwear you may wear. You will usually wear elastic stockings to reduce the risk of blood clots in your legs.
You nurse will attach identity bands to your wrist or ankle and in some hospitals an additional band if you have any allergies.
Premedication (A ‘pre-med’) is sometimes given before some anaesthetics. Pre-meds prepare your body for surgery – they may start off the pain relief, reduce acid in the stomach or help you relax.
A nurse will carry out a pregnancy test on a urine sample if you are of childbearing age. This is standard practice.
You should remove jewellery and/or any decorative piercings. If you cannot remove it, the nurses will cover it with tape to prevent damage to it or to your skin. A wedding ring can usually be worn.
When you are called for your operation
A member of staff will go with you to the theatre, either walking or on a wheelchair/trolley. You can usually wear your glasses, hearing aids and dentures until you are in the anaesthetic room and you may be able to keep them on if you are not having a general anaesthetic.
If you are having a local or regional anaesthetic, you maybe able to take your own electronic device, with headphones to listen to music (check with your nurse beforehand).
Routine checks will be done as you arrive in the operating department, before the anaesthetic starts. You will be asked your name, your date of birth, the operation you are having, whether on the left or right side (if applicable), when you last ate or drank and if you have any allergies. These checks are routine in all hospitals.
Starting the anaesthetic
Your anaesthetic may start in the anaesthetic room or in the operating theatre. Your anaesthetist will be working with a trained assistant. The anaesthetist or the assistant will attach leads to machines to measure your heart rate, blood pressure and oxygen levels and any other equipment as required.
A cannula:
A small plastic tube inserted in your vein with a needle, is used to start most anaesthetics in adults, including a local anaesthetic. All drugs can then be given into your veins using the cannula. If you have any concerns about this, please talk to your anaesthetist.
Local and regional anaesthetics
If you are having a local or regional anaesthetic:
- Your anaesthetist will ask you to keep still while the injections are given. You may notice a warm tingling feeling as the anaesthetic begins to take effect.
- Your operation will only go ahead when you and your anaesthetist are sure that the areais numb.
- You will remain alert and aware of your surroundings, unless you are having sedation. A screen will stop you seeing the operation unless you want to.
- For regional anaesthetics, a member of the anaesthetic team is always near to you and you can speak to them whenever you want to.
General anaesthetics
There are two ways of starting a general anaesthetic:
- Anaesthetic drugs may be injected into a vein through the cannula. This is generally used for adults and is more controlled.
- You can breathe anaesthetic gases and oxygen through a mask, which you may hold if you prefer. After you are unconscious your anaesthetist will put in a cannula.
The Post Anaesthetic Care Unit (PACU)
Also known as the recovery area, is where patients go after surgery if they’ve had general anaesthesia, a spinal, or heavy sedation. Unlike local anaesthesia, which usually allows a direct return to the ward, these procedures require monitored recovery.
Here’s a concise overview based on the details provided:
Purpose and Setup
The PACU is for waking up from anaesthesia or recovering from spinal/sedation effects. Hospitals have multiple PACUs, varying from 3 to 11 bays, with mixed-sex environments hosting patients from different surgeries. You’ll be on a trolley or bed, monitored by specialist recovery staff.
Monitoring and Care
Existing monitoring devices (e.g., for blood pressure, pulse, oxygen saturation) stay attached. You may have a drip or other attachments based on your surgery. Staff ensure comfort and tailor care to your needs, as recovery times vary (30 minutes to several hours).
Visitor and Phone Policy
No family visits or mobile phone use is allowed to protect privacy, as some patients are unconscious or waking up. Provide an up-to-date contact number pre-surgery; staff can call your designated contact if you’re in PACU over an hour to update them (without sharing operation details). Hands-free phones may allow brief patient conversations.
Transfer
Once stable, you’re moved to a ward or, if needed, a high-dependency bed for continued monitoring (pre-discussed by your surgeon/anaesthetist). Delays can be expected based on ward beds availability.
Pain relief after surgery
The type and amount of pain relief you will be offered will depend on the operation you are having and your pain levels after the operation. Some people need more pain relief than others.
Generally, some degree of pain or discomfort should be expected during your recovery. Stronger painkillers can be very good at relieving pain, but may have side effects, like nausea, constipation and addiction in the long term.
Occasionally, pain is a warning sign that all is not well, so you should always report it to your nurses and seek their advice and help.
Here are some ways of giving pain relief:
- Pills, tablets or liquids: To swallow – these are used for all types of pain. They typically take at least half an hour to work. You need to be able to eat, drink and not feel sick for these drugs to work.
- Injections: These may be intravenous (through your cannula into a vein for a quicker effect) or intramuscular (into your leg or buttock muscle using a needle, taking about 20 minutes to work).
- Suppositories: These waxy pellets are put in your rectum (back passage). The pellet dissolves and the drug passes into the body. They are useful if you cannot swallow or if you might vomit.
- Patient-controlled analgesia (PCA): A machine with a push button which, when pressed by you, delivers a small dose of strong pain killer directly into your cannula or drip. It is programmed to ensure you cannot give yourself an overdose. A PCA puts you in direct control of your own pain relief.
- Local anaesthetics and regional blocks: These types of anaesthesia can be very useful for relieving pain after surgery.
Although you may be given a supply of painkillers when you leave the hospital, it is sensible to buy some over-the-counter painkillers to have ready at home. If you are still needing them two weeks after discharge from the hospital, you should get in touch with your GP to discuss this further.
You may go home on morphine-type pain killers following your operation. It is important that you reduce and then stop these medications as soon as possible as their continued use can cause you significant harm.
Risk and anaesthesia
The infographic on the next page shows the common events and risks that healthy adult patients of normal weight face when having a general anaesthetic for routine surgery (specialist surgeries may carry different risks).
Modern anaesthetics are very safe. There are some common side effects from the anaesthetic drugs or the equipment used, which are usually not serious or long lasting. Risks will vary between individuals and will depend on the procedure and anaesthetic technique used.
You and your anaesthetic
Your anaesthetist will discuss with you the risks that they believe to be more significant for you. There are other less common risks that your anaesthetist will not normally discuss routinely unless they believe you are at higher risk. These have not been shown in this leaflet.
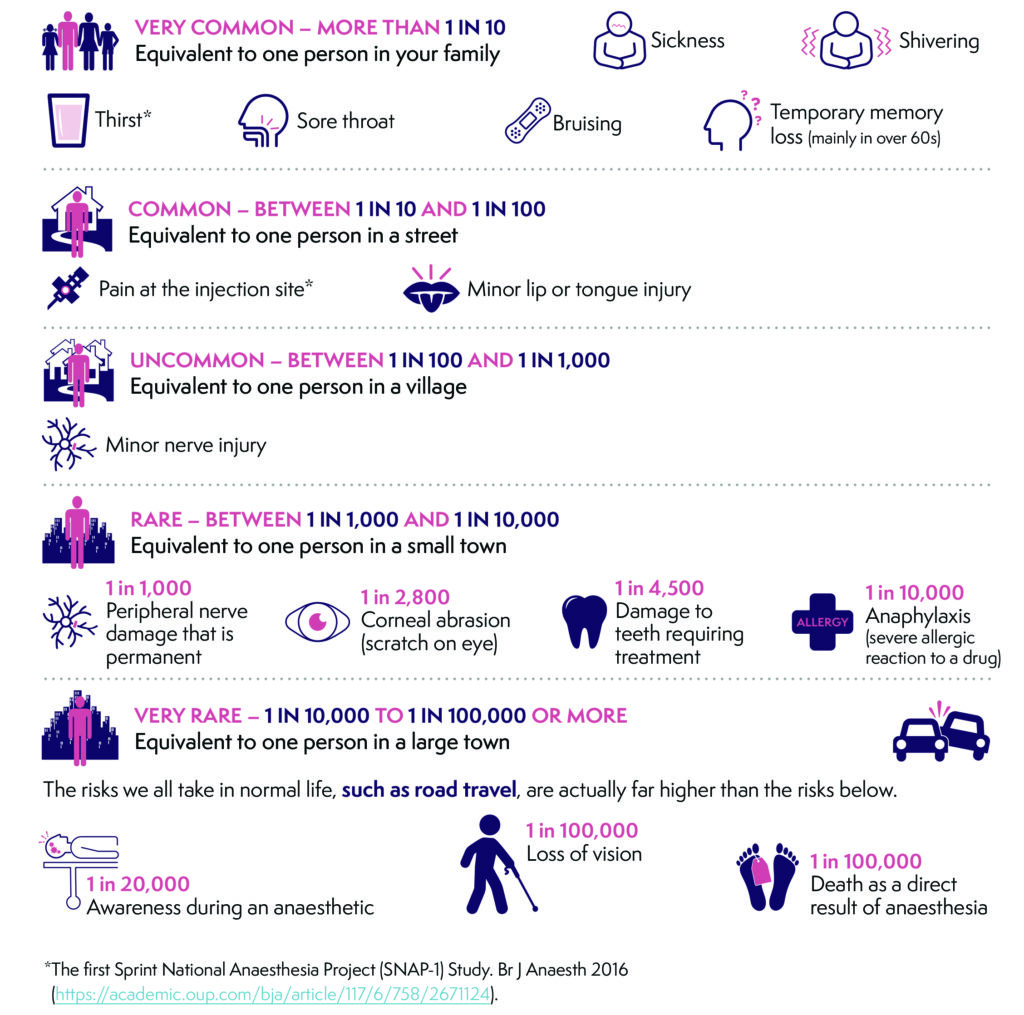
Risks that are very common (more than 1 in 10 people which is the equivalent to one person in your family):
Sickness, Shivering, Thirst*, Sore throat, Bruising and Temporary memory loss (Mainly in people over the age of 60).
Risks that are common (between 1 in 10 and 1 in 100 people which is the equivalent to one person in a street): Pain at the injection site* and Minor lip or tongue injury.
Risks that are uncommon (between 1 in 100 and 1 in 100-people which is the equivalent to one person in a village):
Minor nerve injury.
Risks that are rare (between 1 in 1000 and 1 in 10,000 people which is the equivalent to one person in a small town):
1 in 1000 people may get peripheral nerve damage that is permanent.
1 in 2800 people may get a scratch on the eye (Corneal abrasion).
1 in 4500 people may have their teeth damaged that requires further treatment.
1 in 10,000 people may have a severe allergic reaction to a drug (Anaphylaxis).
Risks that are very rare (between 1 in 10,000 to 1 in 100,000 people or more, which is the equivalent to one person in a large town). The risks we all take in normal life, such as road travel, are actually far higher than the risks below:
1 in 20,000 people may have awareness during an anaesthetic.
1 in 100,000 people may have loss of vision.
1 in 100,000 may die as a direct result of anaesthesia.
*The first Sprint National Anaesthesia Project (SNAP-1) Study. Br J Anaesth 2016
https://academic.oup.com/bja/article/117/6/758/2671124.
Although we try very hard to keep the information in this leaflet accurate and up-to-date, we cannot guarantee this.
This general information will not to cover all of your questions, or deal with everything that might be important to you.
You should discuss your choices and any worries you have with your medical team, using the information in this leaflet as a guide. The leaflet on its own should not be treated as advice.
Tell us what you think
Other sources of information
Many thanks to the Royal College of Anaesthetists & Association of Anaesthetists