Your doctor has recommended that you have a Colonic Stent Insertion. This leaflet will explain the procedure and what to expect on the day of your test. If you have further questions, please ask the nurses or doctors on the ward or discuss them with a member of the Endoscopy staff before your procedure (please see contact details further down this page).
What is a Colonic Stent Insertion?
A colonic stent is a flexible metallic tube, specially designed to open the part of your bowel that is narrowed or blocked due to disease. Once it is in place, the stent is designed to expand and open so that there is a channel for waste products can pass through to reach the rectum. It is difficult to predict how long the procedure will take but usually it takes between 30 and 60 minutes.
Why am I having a Colonic Stent Insertion?
Before the insertion of a colonic stent, other tests such as a CT scan or x-ray have shown that your bowel has become blocked. Your doctor will have discussed with you the likely cause of the blockage. There are different treatments available for people with a blocked bowel but a stent insertion has been proposed as the best treatment option for you. You should make sure that you have had the opportunity to discuss your treatment options with your doctor and if you feel uncomfortable about having a stent inserted, you can decide against it. Your decision will be fully respected and your doctor will be happy to discuss alternative options.
What preparation will I need for my Colonic Stent?
The doctors will advise you of the bowel preparation that you will need for your colonic stent insertion. Sometimes, the doctor may decide that you will require enemas administering to clear the bottom half of your bowel on the day of your procedure.
You will need to wear a gown and remove any tight clothing for your comfort. Please inform the nurse or endoscopists about any allergies or reactions to medications you may have had.
What are the risks of having a Colonic Stent Insertion?
There are six main possible complications directly involved in stent insertion:
- Malpositioning: Occasionally, the size and shape of the blockage makes it impossible to correctly place the stent. In this case, the doctor will stop the procedure and discuss alternative plans with you.
- Migration: The stent may not remain in place, moving either above or below the site of the blockage. In this case, you may experience pain or urgency to open your bowels. Stent migration may require removal and replacement of the colonic stent.
- Perforation: It is possible that the lining of the bowel wall may be torn during the operation. This is an uncommon complication but if it happens, it can be serious and require an operation to resolve the complication.
- Bleeding: A small amount of bleeding is expected but if you are concerned, contact us for advice using the numbers provided at the end of the leaflet.
- Pain: Some discomfort is expected after the stent is placed; however, if your pain is severe, it may indicate obstruction, perforation or migration and please contact us urgently for advice.
- Re-obstruction: Over time, the narrowing may return and block the stent. This may cause pain, vomiting and discomfort. If you develop these symptoms, please contact us urgently for advice. It may be necessary to place an additional stent to relieve this.
Complications may occur in up to 1 in 10 cases. Mostly these will be mild but you may need to remain in hospital for observation or have further treatment. In some cases, complications may be severe, requiring surgery, and rarely these can be life-threatening.
In case of emergency contact 0113 2067833 (nursing co-ordinator number) or out-of-hours, contact switchboard on 0113 2433144 and ask for the gastroenterology registrar on call.
What will happen on the day of the test?
When you arrive at the Endoscopy Unit, your personal details will be checked. The assessment nurse will check your medical history and any allergies. You will be able to ask any questions and discuss any worries or questions that you have about the stent insertion.
What happens in the procedure room?
You will be greeted by two nurses who will remain with you during the procedure. You will be asked to remove any dentures or glasses and lay on your left-hand side with your knees slightly bent towards your chest.
You will be given some oxygen via a small cannula that sits in your nose and your pulse and oxygen levels will be monitored using a probe placed on your finger. Sometimes, we use sedation when stenting a stricture narrowing in the bowel. The drugs used are a combination of a sedative (for example, for Midazolam and Fentanyl) to relax you and a painkiller (e.g. Fentanyl). Occasionally, we also use a drug called Buscopan to relax the bowel. If you are finding the procedure more uncomfortable than you expected, please let the nurse known and you may be given further medication to make you feel more comfortable.
There are known adverse effects from the intravenous drugs administered during the procedure. These range from mild and common (for example, headache, nausea, dizziness) to rare and serious (for example, depression of respiratory and nervous system, which may result in aspiration pneumonia, anaphylaxis and coma. Although these serious complications are rare, they are more common in patients with deeper sedation and/or general anaesthesia.
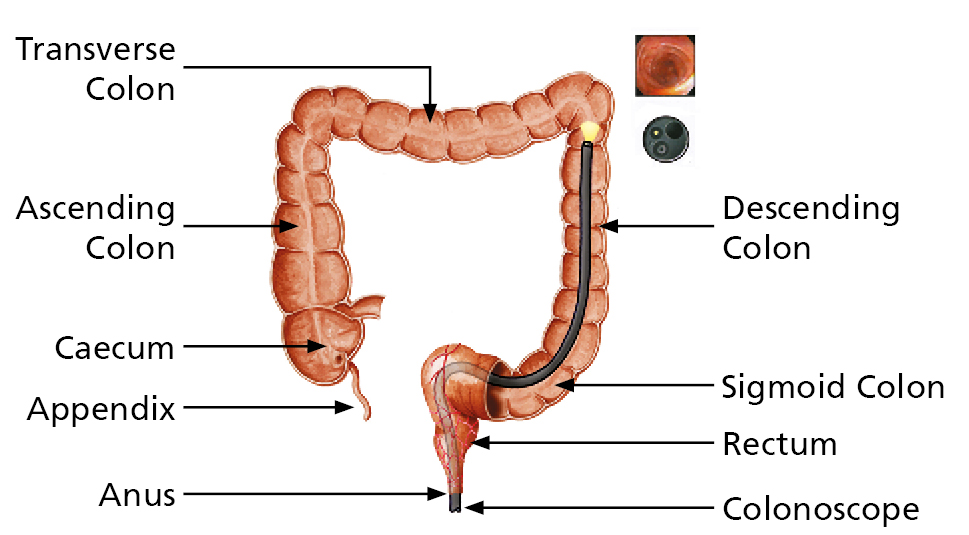
When you are comfortable, a colonoscope (camera) will be passed through your anus into the bowel and then advanced to the area that is narrow through your anus into the bowel. A wire is then passed through the colonoscope and across the narrowed area under x-ray guidance. The stent is then placed over the wire into the correct position.
Please note, all hospitals in the Trust are teaching hospitals. It may be that a trainee endoscopist performs your procedure. However, this will be under the direct supervision of a Consultant experienced in placing colonic stents at all times. You have the right to decline having the procedure performed by a trainee if you wish.
In around 1 in 10 cases, we are unable to correctly position the stent, either because of the angle of the bowel, or because the bowel is not clean enough. If this occurs, the doctor will talk to you about the options at the time.
What happens after the test?
You will be transferred to the recovery room after the test. It is important to tell the nursing staff if you have any pain. You will have your pulse and blood pressure monitored to ensure there have been no complications. You will then return to the ward.
What to expect:
- you may experience some crampy abdominal pain as the bowel returns to normal function; and
- when the bowel is unblocked, it’s normal to develop loose bowels for a few hours. This usually settles after a day or two.
Care following a Colonic Stent Insertion
Your doctor will inform you how soon after the procedure you may eat and drink. It is recommended that you drink plenty of fluids with your meals and that you eat smaller meals more frequently. Try to avoid high fibre foods such as fresh fruit, raw vegetables, fruit or vegetable skins, food with seeds, nuts and tough meats.
You may be prescribed a stool softener and/or laxative.
What should I do if I become unwell after the procedure?
If you experience any unusual pains in the abdomen, not relieved by passing wind or a bleeding from the back passage following your stent insertion, please contact us urgently. Bleeding or perforations can occasionally present several days after the procedure took place.
The stent can also block up with stool at any time. Signs that the stent has become blocked would normally include stomach cramps, nausea and inability to open the bowels.
Please note:
Contact us urgently for advice if you develop any of these symptoms. Remember to tell us that you have a colonic stent.
Please refer to the useful contact numbers below.
Contact numbers:
This leaflet has been designed as a general guide to your test. If after reading this, you have any questions that you feel have not been answered, please contact the Endoscopy department on the numbers on below.