This leaflet provides information about the pregnancy Athena care pathway.
The Athena care pathway is designed for pregnant people with a body mass index of 40 kg/m2 or more at the start of pregnancy and is delivered by specialist midwives.
What is the Athena Pathway?
- The Athena Pathway offers additional pregnancy wellness support, in addition to your community midwife routine appointments.
- The Athena Specialist Midwives provide extra contact points in your pregnancy.
- Extra contact points provide an opportunity to support you with personalised care planning and optimising your health and wellbeing.
Benefits to you
- Additional midwife contact points, support and personalised care by telephone or video call.
- Additional tools and resources to help keep you focused on your health and well-being.
- Additional support to reduce your chances of developing diabetes during pregnancy, high blood pressure and other pregnancy complications.
- Obtain a FREE Active Leeds Pass to access unlimited swim and yoga during pregnancy and post birth in selected community centres and Leeds Council leisure centres around Leeds.
- An opportunity to join midwife-led wellness walks with other pregnant people and new mums.
- An opportunity to connect with other pregnant people and new mums through a dedicated Instagram social media page.
- Feel well, manage pregnancy symptoms and enjoy your pregnancy!
Patient quote:
“I found the conversations sensitive and super empowering. I loved that I could have midwifery-led care”
Diane, first time mum
Flow Chart
This flow chart shows the Athena pathway appointment schedule and is in addition to your normal community midwife care appointments:
1. Initial booking

- After booking with your community midwife, an Athena midwife will contact you, usually within a week by telephone.
2. Initial contact
- Telephone contact from an Athena midwife around 1-2 weeks after your booking appointment to introduce the Athena pathway.
- Discussions will include:
– Healthy eating, self-care and keeping active in pregnancy.
– Introduction to the free Active Leeds offer and relevant living resources.
3. 2nd Athena Pathway contact
- Telephone or video call contact from an Athena midwife between 14-18 weeks of pregnancy. Discussions will include:
- Ongoing personalised wellness support and information and resources on pregnancy vitamins, vaccinations and self-care.
4. 3rd Athena Pathway contact

- Telephone or video call contact from an Athena midwife between 21-24 weeks of pregnancy. Discussions will include:
- Review of personalised wellness plan and how this can continue to the end of pregnancy.
- Anaesthetic team referral offer if applicable, connecting with like-minded peers, baby movements in pregnancy, antenatal education classes and feeding your baby.
Reminder
Remember Athena pathway care is additional to your regular pregnancy care. We recommend continuing to attend routine pregnancy care with your community midwife and any additional scans or appointments you are offered by the hospital.
Additional care offers
- Additional growth ultrasound scans will be offered at 32 and 36 weeks and possibly 39 weeks as required.
- A blood sugar test will be offered to check for chances of developing diabetes in pregnancy at 26-28 weeks. If you have had Gestational Diabetes before, this test will be offered earlier around the time of your dating scan.
- Moving and handling assessments may be offered by an Athena midwife around 36 weeks of pregnancy to assist with safe birth planning.
Initial Athena Pathway Contact
(1-2 weeks after your booking appointment)
1. What we’ll talk about
- Optimising pregnancy wellness for you and your baby.
- Supporting your mind and body: Eating well, movement, sleep, vitamins, self-care and relaxation.
- What’s important to you: We’re here to support you and talk about any worries or issues you might have.
- Other care offers such as:
- Blood Sugar Test to check for diabetes in pregnancy.
- Low Molecular Weight Heparin Injections if indicated
Your upcoming appointments: Details about your next Athena appointments in your pregnancy.
Pregnancy Wellness Class Transcript
I’m Anna. I’m a midwife working at Leeds Teaching Hospitals Trust, and we’ve designed a Pregnancy Wellness class to help manage some of the symptoms you may—or may not—develop as your pregnancy progresses.
This class recording is ideally watched towards the end of the first trimester or into the second trimester, but you can watch it at any time. It may still be of help. The session takes around an hour.
I’m going to share my screen shortly and take a top-to-toe approach to the symptoms you might experience, with a focus on nutrition and movement, which are often our first line of defence. Please feel free to get comfortable, grab a warm or cold drink, and perhaps a pen and paper so you can take notes throughout.
Welcome to your Second Trimester Top-to-Toe Wellness Class. Don’t worry if you’re still in the first trimester or if you’re watching this in the third trimester—it may still be of great benefit.
Today we’ll cover:
Supporting your emotions and mental health
Improving sleep
Oral health
Pregnancy cravings
Supporting your immune system
Iron intake and supplementation
Baby movements and patterns
Managing constipation and acid reflux
Pelvic girdle discomfort
Building healthy habits
Available support
Nutrition and movement are often our first line of defence and support.
Activity in Pregnancy
A quick recap on activity levels in pregnancy: we recommend 150 minutes of moderate physical activity per week. Moderate activity means moving to the point where you feel slightly breathless but can still hold a conversation.
Benefits of regular movement include:
Reduced risk of gestational diabetes
Improved mood and sleep
Lower blood pressure
Reduced excessive weight gain
Improved fitness for labour and birth
Activities can include walking, housework, gardening, dancing, and playing with children—all of these count.
If you’re not currently exercising, start gradually with 10-minute sessions and build up. Making small swaps, such as taking the stairs instead of the escalator, can help incorporate movement into your routine.
Twice weekly, aim to include muscle-strengthening activities. These don’t have to involve weights—walking uphill, stairs, cycling, Pilates, and pregnancy yoga all help strengthen the core muscles used during pregnancy, labour, and recovery.
Listen to your body. If you experience pain, stop and restart gently. For persistent pain, contact your GP or maternity assessment centre. Adapt activity as pregnancy progresses—brisk walking is often a great option.
Nutrition in Pregnancy
Movement and good nutrition work together. Regular movement can ease aches, pelvic discomfort, and help control blood sugar and blood pressure, improve sleep, and support mental health. Nutrition supports energy levels, mood, skin and hair health, and healthy weight gain.
Use the Eatwell Guide as a visual reminder:
Fruit and vegetables: at least half your plate (fresh, frozen, or tinned)
Starchy carbohydrates: just over one third (choose wholegrain where possible)
Protein: beans, pulses, fish, eggs, lean meat
Dairy: milk, cheese, yoghurt (choose plain options)
Healthy fats: nuts, seeds, avocado, olive oil
Foods high in sugar, salt, and saturated fat should be limited and are best considered occasional treats.
Be mindful of drinks—full-sugar fizzy drinks, fruit juices, and sweetened hot drinks can contain hidden calories and sugar. Reduce caffeine to no more than 200 mg per day. Avoid alcohol entirely.
Foods to Avoid in Pregnancy
Avoid:
Unpasteurised milk and dairy products
Mould-ripened soft cheeses (unless cooked until piping hot)
Undercooked meat, liver, and pâté
Game meats
Cold cured meats unless thoroughly cooked
Lion-stamped eggs are safe to eat runny. Eggs without a lion stamp should be fully cooked.
Avoid high-mercury fish such as shark and swordfish. Limit oily fish to two portions per week. Cooked shellfish is safe.
Nuts and seeds are encouraged unless you have an allergy. Eating nuts in pregnancy may reduce your baby’s risk of developing nut allergies.
Emotional Wellbeing and Sleep
Pregnancy hormones can cause emotional highs and lows, including anxiety, excitement, fear, joy, and overwhelm. Poor sleep and vivid dreams are common.
Tips for better sleep include:
Keeping the bedroom cool and ventilated
Avoiding heavy meals close to bedtime
Using pillows for support
Avoiding lying flat on your back
Movement, especially outdoors, mindfulness, breathing exercises, journaling, and talking to your support network can all help support mental health.
Always tell your midwife how you’re feeling emotionally—support is available.
Immunity and General Health
Your immune system is lower in pregnancy. Support it by:
Eating a varied diet rich in fruit and vegetables
Drinking at least 2 litres of water daily
Reducing sugar and processed foods
Taking daily vitamin D
Flu and COVID-19 vaccinations are offered during pregnancy and are recommended.
Cravings
Cravings are common and often ease later in pregnancy. Non-food cravings (such as ice, clay, or soap) should be reported to your midwife, as they may indicate iron deficiency.
Aim for balance and moderation.
Smoking and Vaping
Stopping smoking before 16 weeks reduces risks significantly. Smoking increases the risk of miscarriage, stillbirth, premature birth, and low birth weight.
Vaping is considered safer than smoking if used as a quitting aid. Leeds Teaching Hospitals’ Stop Smoking Service can provide support and nicotine replacement therapy (avoid liquorice-flavoured products).
Oral Health
Hormonal changes can cause bleeding gums. Brush twice daily, floss, and use mouthwash. Use your FW8 exemption for free dental care during pregnancy and until your baby is one year old.
Acid Reflux
Common in pregnancy due to hormonal relaxation of the stomach valve. Helpful strategies include:
Avoiding fizzy, fatty, or greasy foods
Staying upright after meals
Eating slowly
Avoiding meals close to bedtime
Medications such as Gaviscon or prescribed treatments may be used safely—speak to your GP or midwife.
Iron and Anaemia
Iron is essential for oxygen transport. Symptoms of anaemia include fatigue, dizziness, breathlessness, and paleness.
Increase iron intake through leafy greens, beans, red meat, nuts, seeds, and fortified cereals. Iron supplements may be prescribed if needed. Some women require iron infusions.
Baby Movements
Movements are usually felt between 16–20 weeks. Patterns develop from 28–32 weeks. Always contact your maternity assessment centre if movements reduce or change.
Do not use home Dopplers.
Pelvic Girdle Pain and Pelvic Floor
Pelvic discomfort is common and can be managed with physiotherapy, gentle exercise, support belts, and good posture.
Pelvic floor exercises are recommended daily. Use the NHS Squeezy App for guidance.
Swelling and Urinary Symptoms
Swelling is common later in pregnancy but sudden swelling with headaches or visual changes needs urgent assessment.
Urinary tract infections are more common—report burning, pain, fever, or back pain promptly.
What’s Next
Expect:
Anatomy scan at around 20 weeks
Midwife appointments from 25–28 weeks
Whooping cough vaccination from 20–32 weeks
Blood tests at around 28 weeks
MATB1 form for work
Focus on self-care, regular movement, good nutrition, and rest.
Thank you for joining this session. We hope it has helped you understand how to manage pregnancy symptoms and feel supported. We’d love your feedback, and we look forward to welcoming you to our next class on preparing for labour, birth, and meeting your baby.
Please keep looking after yourself.
Patient quote:
“The Athena Midwives supported me throughout pregnancy with keeping active- they helped me to stay motivated which helped me control my weight gain”
Jenna, Leeds
2nd Athena Pathway Contact
(Between 14-18 weeks of pregnancy)
1. What we’ll talk about
- How You’re Feeling: We will ask you about your physical and emotional wellbeing, offering support with any lingering pregnancy symptoms.
- Pregnancy Progress: How your pregnancy is going and answer any questions you may have.
- Your wellness journey: We will review your wellness and self-care plan.
- Stress & Self-Care Tips: Share ways to manage stress, sleep well and take care of yourself.
- Wellness Tips: Discuss how to keep moving, eat well and take time to reflect.
2. Next Steps
- Book Your Appointment: Schedule your next Athena pathway contact in.

3rd Athena Pathway Contact
(Between 21-24 weeks of pregnancy)
1. What we’ll talk about
- Preparing for later stages of pregnancy and birth: As you enter the final stretch of your pregnancy, focus on winding down, resting and relaxing.
- Scan Results: Chat about how your routine scan went and offer additional scans as necessary.
- Discuss any worries and extra support you may need.
2. Continued self-care discussions
- Healthy Habits: Focus on eating well, adapting activities to your stage of pregnancy, and relaxation techniques to feel good.
- Managing Stress: Learn ways to handle stress and get ready for your baby with positive birth affirmations.
- Baby Preparation: Learn about and discuss feeding your baby, activities you can do with your baby and post birth support.

What are the benefits of being active in pregnancy?
- Keeping active keeps both you and your baby healthy
- Helps control weight gain.
- Helps prevent diabetes in pregnancy.
- Improves sleep.
- Helps to maintain a healthy blood pressure.
- Helps boost your mood and mental well-being.
- Helps recovery post-birth.
Daily moderate intensity physical activity means doing activities that make you breathe faster and feel warmer, but you can still talk without too much difficulty.
Examples include brisk walking, carrying light shopping bags, swimming, household chores, cycling at a moderate pace, or dancing. It’s a good way to stay healthy and active during pregnancy, and great to do with friends and family.
Join us on wellness walks to meet other pregnant women and get moving socially.
Active Leeds
- Offers free pregnancy and postnatal yoga classes in community and leisure centres across Leeds.
- Provides Bump and Baby Fit sessions before and after birth, plus free swimming during pregnancy and up to one year post-birth at Leeds City Council Leisure Centres.
- Runs parent/carer and baby yoga sessions in selected community centres.
Useful information on physical activity during pregnancy
Pelvic Floor Health
What is the pelvic floor?
- The pelvic floor consists of layers of muscles that stretch like a supportive hammock from the pubic bone (at the front) to the tailbone (coccyx) at the back.
Why is it important to train the pelvic floor muscles?
- Pelvic floor muscles help to support your bladder, bowel and vaginal function.
- There is high quality evidence that it is important to take care of your pelvic floor muscles in pregnancy.
- If your pelvic floor muscles are weak, you may find that you leak urine when you cough, sneeze or strain.
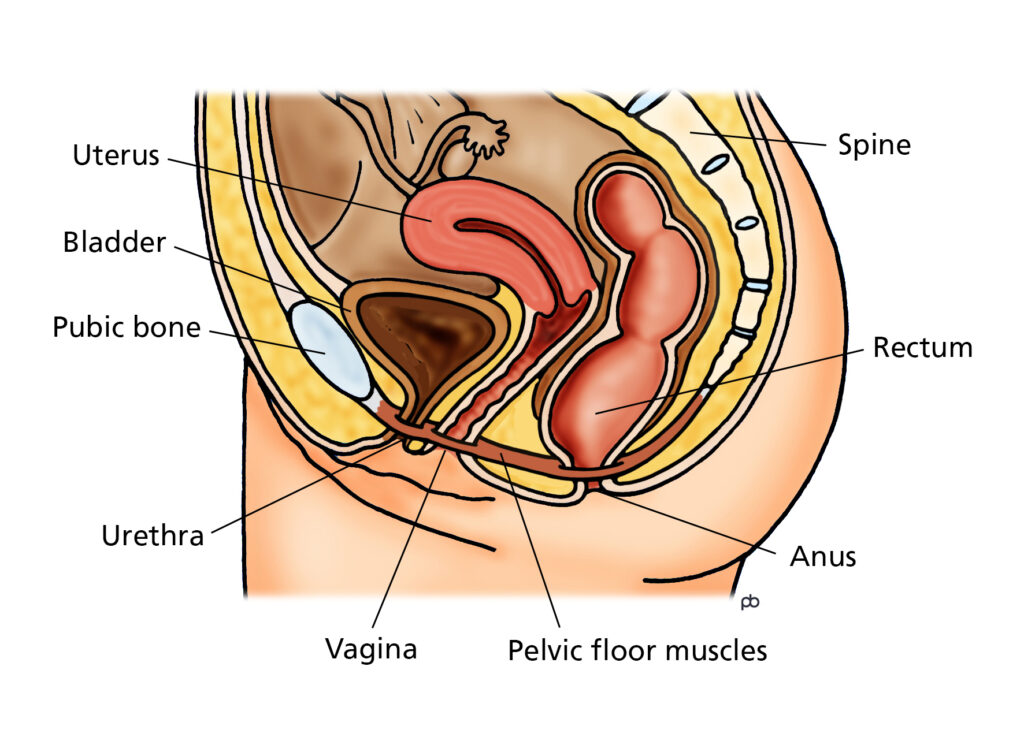
Pelvic floor muscle training
Easy steps for pelvic floor muscle training:
- Find the Right Muscles: To locate your pelvic floor muscles, engage your back passage imagining you are stopping yourself breaking wind, followed by engaging your front passage as if you are stopping yourself passing urine. You should feel a lift and tightening sensation in your vaginal region.
- Practice the Squeeze: Tighten your pelvic floor muscles for up to 10 seconds, then relax for the same amount of time.
- Repeat: Aim to complete these long squeezes 10 times, followed by 10 quick 1 second hold repetitions. You can do this while sitting, standing, or lying down.
- Focus: Make sure to only tighten your pelvic floor muscles, not your stomach, thighs, or buttocks. Breathe normally during the exercises.
Visual Guide
Healthy Eating
- Eating well during pregnancy supports both you and your baby’s health.
- The NHS Eatwell Guide is a visual tool that shows you how to eat a balanced diet by including different foods from each food group:
– Fruits and vegetables: for vitamins, minerals and fibre
– Starchy foods: like bread and rice for energy
– Proteins: like meat and beans to build and repair body tissues
– Dairy and alternatives: for strong bone development.
– Small amounts of oils and spreads: for healthy fats.
Eating well tips
- Eat a Variety: Fill your plate with lots of fruits and vegetables.
- Add Nuts and Seeds: They’re great for protein and healthy fats (avoid if allergic)
- Limit Sugar and Carbohydrates: Keep carbs to about a third of your meal and limit foods with added sugar such as cakes and sweets.
- Meal Prep: Prepare meals ahead of time, batch cook and try easy homecooked recipes.
- Portion size: Eating for two during pregnancy is a common myth. Your body needs good quality nutrients rather than extra calories to support your baby’s growth.
- Drink Swaps: Avoid alcohol and limit caffeine to 200mg per day throughout pregnancy. Decaffeinated tea and coffee can be a good swap.
Food Safety
Healthy Start Scheme
Get financial support to buy fruits, vegetables, pulses, milk and vitamins.
What is NHS Healthy Start?
Healthy Start provides financial support to pregnant people and families on a low income to help them access fruits, vegetables, pulses, milk and get the vitamins needed for healthy development.
You may qualify for Healthy Start vouchers if you’re at least 10 weeks pregnant or have a child under four years old and are also in receipt of certain benefits.
What do I receive?
If eligible, you can get payments every 4 weeks to spend on:
- Cow’s milk
- Fresh, frozen or tinned fruit and vegetables
- Infant formula milk based on cow’s milk
- Fresh, dried, and tinned pulses
You can also get free Healthy Start vitamins.
Tips for eating healthy on a budget
- Frozen and Canned Options: Frozen and canned fruits and vegetables are often cheaper and last longer, making them cost-effective options.
- Buy in Bulk: Items like rice, pasta, and beans are often cheaper when bought in bulk.
- Batch Cooking: Prepare large portions of meals and freeze them for later use.
Preparing for later pregnancy and birth
Final Tips for the Third Trimester
- Rest and Activity: Prioritise rest and gentle activities like walking or swimming.
- Birth Plan: Think about your birth plan but stay flexible.
Antenatal Appointments and Maternity Rights
- Paid Time Off: You’re entitled to paid time off for pregnancy-related appointments, including scans, health checks, and classes like Active Leeds Bump and Baby Fit.
- Employer Letter: If needed, a letter for your employer can be provided to confirm your right to time off.
Anaesthetic Information
Whether you are considering having an epidural or not for pain relief during birth, this video link from our local Anaesthetic team may help to answer questions you may have on anaesthetic pain relief options, when they may be offered and the role of the anaesthetic team during birth.
You may be offered a consultation with the Anaesthetic team during the later stages of pregnancy to inform birth planning.

Pregnancy and Birth Information Resources
- Labour and birth preparation video: Topics Covered: Hormones and stages of labour, pain relief options, different birth modes (vaginal, caesarean, assisted births), tips for birth partners, and what to expect after birth.
Labour and Birth Preparation transcript
My name’s Anna. I’m one of the midwives working at Leeds Teaching Hospitals, and I work in the Health and Equity Team. We’ve put together a presentation to help you better prepare for the labour and birth of your baby.
The presentation is about an hour in length. We’ll remind you at the halfway mark to pause, have a break, or have a shuffle, but of course, because this is recorded, you can pause and take breaks as many times as you want. You might want to consider having your birth partner, or both partners, watching this together. You can make notes throughout, or do both.
The most important thing is to get comfortable. Maybe have a drink beside you as we go along. I’m going to share my screen in a second and talk through some slides that should be really helpful as you prepare your body and mind for your journey of labour and birth ahead.
Welcome
In today’s session we’ll discuss:
The hormones that drive labour
The signs and stages of labour
What happens during labour and when to call the hospital
Different modes of birth that may be offered and encouraged, including vaginal and assisted birth
All pain relief options
The benefits of active birth
The benefits of being an active birth partner
The immediate moments after birth with your baby
Hormones that drive labour
Oxytocin is a wonderful “love hormone” and drives your entire labour. You can’t labour without this hormone. Higher oxytocin levels are associated with smoother and quicker labours. It’s a private and romantic hormone, and it’s the same hormone we produce when we’re falling in love.
Oxytocin increases when you feel safe and loved. You can boost it by staying close to your birth partner, surrounding yourself with your favourite things, and keeping as relaxed and calm as possible throughout labour. This hormone loves soft lighting and privacy. What can you think of that would help increase your oxytocin levels during labour?
Adrenaline, in comparison, can interfere with labour if produced in high amounts. This is the hormone we want to keep low so oxytocin can rise again. You can help reduce adrenaline by keeping your favourite things close and feeling safe.
Endorphins are another helpful hormone produced during labour. These naturally occurring hormones act as your body’s own painkillers, reducing your perception of pain and helping to comfort you throughout labour.
When does labour happen?
Do you think most babies are born on their estimated due date? Is that true or false?
It’s false. Only around 3–5% of babies are actually born on their due date. You’re likely to go into labour anytime between 37 and 42 weeks of pregnancy. Sometimes, if there are no signs of labour, you may be offered an induction.
Can anyone think of a sign of labour?
The three main signs of labour are:
Losing your mucus plug
Your waters breaking
Contractions starting
Mucus plug
The mucus plug forms a seal to prevent infection and bacteria entering the uterus during pregnancy. It may come away towards the end of the third trimester or during labour. You may or may not see it. It can be slightly bloodstained, which is normal.
If you lose your mucus plug before 37 weeks, especially if you experience lower abdominal or back discomfort, this could be a sign of premature labour. You should call the maternity assessment centre.
Waters breaking
For around a quarter of women, waters breaking is the first sign of labour. They are usually clear or pink. They may come as a trickle or a gush. However, they can also be green, yellow, or brown, which may indicate your baby has passed meconium (their first poo) inside the womb.
For most women, labour starts within 24 hours after the waters break. If labour doesn’t begin within that time, an augmentation (a process to speed things up) may be encouraged. This could include your midwife breaking your waters if labour is slow, or as part of an induction.
If you think your waters have gone, call your maternity assessment centre and place a thick maternity pad in your underwear.
Contractions
For around three-quarters of women and birthing people, contractions are the first sign of labour. They usually begin between 37 and 42 weeks.
Contractions are powerful squeezes around your baby. The muscles at the top of the uterus contract and shorten, pushing your baby onto the cervix. This causes the cervix to lift, soften, shorten, and open.
You may feel lower abdominal discomfort, back pain, or both, increasing in strength and length over several hours. Your hormones drive these contractions throughout labour.
Stages of labour
Labour can be divided into three sections: the beginning, the middle, and the end.
Early labour is generally from 0–4 cm dilation. The cervix gradually softens, lifts, and opens. This process may stop and start and can take hours or even days.
Active labour is usually between 4–8 cm. The cervix continues to open as your baby’s head moves deeper into the pelvis. With a first baby, the cervix often opens at an average rate of about 1 cm every 2 hours from this point.
Transition occurs between 8–10 cm. This phase can involve a surge of adrenaline, making you feel restless or agitated. It’s often short-lived. You may feel increasing rectal pressure as your baby moves very low in the pelvis.
The final stage is the pushing stage, where your baby is born.
Monitoring during labour
Monitoring is offered throughout labour. In early labour, you may be at home, observing baby’s movements, contraction patterns, and the colour of your waters. If you’re in hospital, particularly for an induction, you may be offered closer monitoring via CTG.
Blood pressure, pulse, and temperature checks are usually taken every 4–6 hours early on. In active labour, vaginal examinations may be offered every 4 hours to assess cervical change, or sooner if there are concerns. Continuous observation of your contractions, baby’s movements, and the colour of your waters also takes place.
Perineal massage
Perineal massage can be helpful if you’re planning a vaginal birth. The perineum is the skin between the vulva and the anus, which stretches during birth.
Research shows that starting perineal massage from around 34 weeks, three to four times a week for 3–4 minutes, can reduce more severe tearing. You’ll need clean hands, short nails, and a non-irritating oil.
You can gently insert two fingers or thumbs about 2 cm into the vagina, applying downward pressure and gently moving side to side. It should feel uncomfortable but not painful. Partners can help if you’re comfortable with that.
Vaginal birth and assisted birth
Most babies are born vaginally without assistance. Towards the end of labour, your baby’s head will crown at the perineum. You’ll be encouraged to breathe your baby out gently. Your midwife or obstetrician may use a hands-on technique, with your consent, to reduce perineal trauma.
Babies can be born on land or in water and are ideally placed straight onto your chest for skin-to-skin contact.
Some births require assistance, such as forceps or ventouse (suction cup). These are performed by obstetricians, with appropriate pain relief and consent. An episiotomy may be offered if needed, again only with consent.
Water birth
Water birth is considered safe for many women. It’s usually suitable when:
Baby is head down
There is one baby
Labour is progressing normally
There are no pregnancy complications
You can labour in water and birth on land, or labour and birth in water. You don’t need to book a water birth in advance—just discuss it when you attend maternity assessment.
Caesarean section
A caesarean section can be planned or performed as an emergency. Planned caesareans usually happen around 39 weeks. Emergency caesareans can occur if there are concerns about baby or labour progress.
A spinal anaesthetic is commonly used. After surgery, you’re usually mobile within 4–6 hours. A urinary catheter is placed temporarily. Hospital stay is usually around 24 hours.
Pain relief, wound care, nutrition, hydration, and support at home are important for recovery.
Birth of the placenta and delayed cord clamping
The placenta is always born after your baby. This can happen naturally or with an injection to reduce blood loss. Delayed cord clamping is standard practice and allows valuable blood, oxygen, and stem cells to pass to your baby.
When to call the hospital
Call the hospital if:
You think your waters have broken
You have signs of labour before 37 weeks
Contractions are every 5 minutes, lasting 1 minute, for at least an hour
Active birth and pain relief
Being upright and mobile helps labour progress. Gravity is your friend. Props such as birth balls, peanut balls, stools, and the bed can all help.
Create a “toolbox” for labour:
Breathing techniques
Movement
Water
Heat
Music
Aromatherapy
TENS machine
Affirmations
Food and drink
Hospital pain relief options include gas and air, morphine, epidural, and spinal anaesthetic.
Role of the birth partner
Your birth partner is a form of pain relief. They help keep you calm, mobile, hydrated, nourished, reassured, and supported. The “UMBRELLA” approach includes:
Upright
Mobile
Breathing
Resting
Eating and drinking
Loving support
Encouraging toileting
Asking questions
The golden hour
The hour after birth is known as the golden hour. Skin-to-skin contact helps regulate baby’s temperature, blood sugar, feeding, bonding, immunity, and oxytocin levels. Vernix on baby’s skin is normal and protective.
Postnatal care and recovery
Recovery varies for everyone. Focus on nutrition, hydration, rest, pain relief, wound care, and support. Contact your midwife if you notice increased pain, discharge, smell, redness, or feel unwell.
Final thoughts
We hope this presentation has been helpful and given you food for thought. Write down any questions to discuss with your midwife. Consider affirmations, playlists, relaxation techniques, and a birth preference plan.
Thank you for watching. Please share feedback and questions with your community midwife. Good luck, and congratulations in advance on the birth of your baby.
- Preparing for Birth and Beyond (PBB): are free local online and in-person antenatal education classes.
- Preparing to Breastfeed: this class gets wonderful feedback and is well attended. Even if you are planning to formula feed your baby, knowledge on the microbiome and tips on colostrum harvesting may be of great benefit to you and your family!
Health and Wellbeing after Birth
- 6-8 week post birth GP appointment: This is a routine offer to all with the aim to assess your physical and emotional well-being, discuss healing from birth, address any concerns, and provide guidance on contraception, post birth recovery. If you are overdue a cervical smear due to pregnancy – you can arrange a future day for this too.
- You can get pregnant as little as 3 weeks after the birth of a baby. If you have birthed your baby by Caesarean Section, it is generally recommended to have a period of between 12-18 months before trying for another baby- to allow a longer time for the scar on your uterus to heal fully. Information on sex and contraception choices after birth can be found on the NHS website.

Post Birth Health
After the birth of your baby, it is important to continue to eat a healthy, balanced diet to support post birth recovery and an ongoing healthy lifestyle.
Regular, moderate movement post birth is known to reduce your chances of developing type 2 diabetes, high blood pressure and cardiovascular disease.
It can also help you to lose weight and feel more energised improving mental wellbeing.
A healthy weight in a future pregnancy can help reduce your chances of experiencing a miscarriage and stillbirth or developing pre-eclampsia and/or gestational diabetes.
- Pelvic floor exercises: after birth can help aid recovery, reduce incontinence and even help sex to feel better!