You will receive this leaflet if your baby is found in the breech position.
What does breech mean?
A breech presentation is when the baby’s head is at the top of the womb and it’s bottom will be delivered first. There are several different types of breech presentation and the pictures below, show the various ways the baby may be positioned. The most common type is the frank / extended breech, where the legs are straight against the body.
Types of breech position
Extended or frank breech
The baby is bottom first, with the thighs against the chest and feet up by the ears. Most breech babies are in this position.
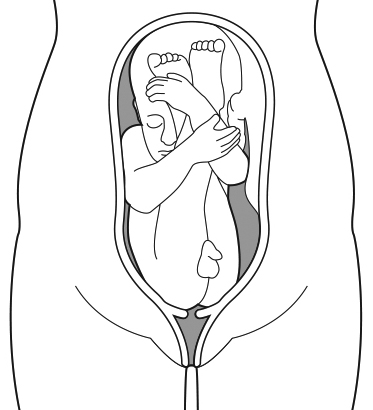
Flexed breech
The baby is bottom first, with the thighs against the chest and the knees bent.

Footling breech
The baby’s foot or feet are below the bottom.

Breech presentation is common in early pregnancy but most babies turn themselves around into head first position before the time of delivery. Three in every 100 babies are breech at the end of pregnancy. This happens more frequently in first time mums.
We know that after 36 weeks of pregnancy, only 6 percent of breech babies will turn into the head-down position on their own.
What next?
If your baby is found to be breech any time after 34 weeks, the health care professional will refer you to the breech clinic, where you will be seen by a midwife who will talk to you about all of your options.
Please note –
If you have already made the decision to have a caesarean section, then you will not be referred to the breech clinic.
At your appointment in the breech clinic, the midwife will discuss different ‘natural’ ways to turn your baby, which you can do at home between 34 and 36 weeks. You will then be seen back in the breech clinic at around 36 weeks to see if your baby has turned. If your baby is still breech then the midwife will discuss having an ECV (external cephalic version – this will be explained further in this document), ideally between 36-37 weeks, but can be done any time up until 40+ weeks.
In some cases, you might find out your baby is breech after 36 weeks. This just means you won’t be referred to the breech clinic, and there are 3 main options if your baby is breech from 36 weeks onwards:
- To have an external cephalic version (ECV).
- To have a planned caesarean section from 39 weeks.
- To plan for a breech vaginal birth.
Vaginal breech delivery can be more complicated than cephalic (head-down) delivery. However, performing a caesarean section poses risks associated with having an operation, and can increase the risk to future pregnancies. For these reasons we offer ECV, which aims to turn the baby into the head-down position before labour, to give a better chance of a normal vaginal delivery. Prior to having an ECV you will need to have a detailed ultrasound scan to measure the baby’s growth, check the fluid around the baby and the position of the placenta.
How is ECV done?
ECV is usually done on the Antenatal Day Unit where the baby’s heart can be monitored on a Cardiotocograph (CTG) machine. You will be offered a small injection of medicine called Terbutaline to help relax the womb to help turn the baby; this medication is safe for the baby. Using a lubricant, the doctor / midwife will place their hands on your abdomen and push to encourage the baby to turn into the cephalic (head-down) position.
Will ECV be successful?
Success rates are usually quoted around 50%, but in Leeds around 2 out of 3 (67%) of ECVs are successful. Success rates are slightly higher if it is not your first baby. There is a 1 in 20 chance that after successful ECV the baby may turn back to breech.
When should an ECV be done?
The best time is 36-37 weeks of pregnancy, but it can be done any time after this, including in early labour.
Is ECV safe?
ECV is a safe procedure and your baby will be monitored throughout. ECV can be uncomfortable, but rarely has to be stopped due to pain. If you are not able to tolerate ECV, the procedure can be stopped at any time. In the unlikely event that the baby becomes distressed, you will be transferred to Delivery Suite for a full assessment. Research shows that in one in 250 cases, delivery by emergency Caesarean section was required after having ECV.
There are very few reasons an ECV should not be offered. For example, it is safe to do if you have had a previous caesarean section, if your baby is thought to be smaller or bigger and if there is less or more than normal amounts of fluid around the baby. ECV is safe whichever of the breech positions your baby is in. If your baby is transverse (lying across) then sometimes an ECV is offered, or sometimes it may be better to wait to see if the baby turns itself to head down.
What happens after the ECV?
After the ECV, the baby’s heartbeat will be monitored using the CTG machine for about 20 to 30 minutes. If your blood group is Rhesus negative and your baby is thought it be Rhesus positive, you will need to have an injection of Anti-D.
If the ECV is successful, we will arrange a presentation scan for you a week later to make sure baby remains head down. If the ECV is unsuccessful, then there may be the option to have a second attempt at ECV on a different day. Alternatively, a caesarean section can be planned (usually at 39 weeks). A vaginal delivery is also usually appropriate, but this will need a more detailed discussion to individualise the information depending on your circumstances. It is important to consider this information carefully even if planning a caesarean section as labour can occur before this point. This discussion should take place with an obstetrician.
All babies that are found to be breech at 36 weeks onwards should be referred for a hip scan after they are born as they are at a small increased risk of hip dysplasia. This should be arranged before discharge after the baby is born, and should be done whether the baby is born vaginal or by caesarean section, and whether it is breech or cephalic when born.
At home after ECV
If you have any bleeding, abdominal pain, contractions or reduced baby movements, please contact the Maternity Assessment Unit straight away.
Where can I get more information?
Do not hesitate to ask your doctor or midwife if you have any further questions. Our policies are in accordance with the Royal College of Obstetricians and Gynaecologists guidelines which can be found online.