We hope this information will help answer any questions you may have. The printed copy and downloadable PDF also contain a treatment diary to help you to remember to take your medication. Use the diary to record any side-effects that you may experience or questions you may have about your treatment.
Please ask your doctor or nurse if you have any questions or concerns.
How does Capecitabine work?
Capecitabine is a tablet you swallow which is then absorbed into the blood stream. Capecitabine may stop cancer cells from growing, causing the tumour to shrink or disappear.
How should I look after my Capecitabine tablets?
- As Capecitabine is a chemotherapy drug always wash your hands thoroughly before and after handling the tablets.
- Capecitabine should be stored in a cool dry place at room temperature.
- Never share Capecitabine with anyone; it has been prescribed for you personally.
- Keep this and all other medicines out of the reach of children.
- If you or someone else takes Capecitabine by accident, or you take more than the prescribed dose, contact St. James’s University Hospital immediately.
Please use the number you have been given to contact the oncology bleepholder for advice.
Special care when taking capecitabine:
- Flush the toilet twice after use with the lid down.
- Everyone should urinate sitting down.
- Please use gloves when cleaning up any spillage of waste products (urine, diarrhoea or vomit)
How to take Capecitabine tablets
The Capecitabine tablets come in two strengths:
150mgs and 500mgs tablets.
Your hospital doctor will prescribe your Capecitabine in treatment cycles. In each cycle, you will take your capecitabine tablets twice a day. You may have to take a combination of both strengths of tablets. This is calculated using your height and weight. It will be clearly written on the boxes of tablets how many you will need to take and the pharmacist or nurse will explain this to you.
Your doctor or nurse will explain how many days you need to take the tablets for. You may have a rest period, when you do not take your capecitabine tablets. This will be explained to you.
- Take the tablets in the prescribed combination, each morning and night.
- We suggest you take the Capecitabine tablets 12 hours apart, for example 9am and 9pm.
- Capecitabine tablets should be taken within 30 minutes of eating a meal or snack.
- Do not chew or crush the tablets.
- Take the tablets with water.
- If you have problems swallowing tablets you can dissolve the capecitabine tablet in warm water. They may taste bitter so adding orange juice can help them taste better.
- If you have any capecitabine tablets left over please return them to the hospital.
What if I miss a dose?
If you miss a dose only take your regular dose at the next scheduled time. Don’t double up the next dose to try to make up for the dose missed. If you are sick and think you may have vomited the tablets back up, do not take the dose again or double up your next dose.
Taking other medicines with Capecitabine
You should inform your doctor or nurse at the hospital about any other medicines you are taking or plan to take before starting capecitabine. This includes prescribed medicines and those you get without a prescription including herbal or vitamins.
This is very important as taking some medicines at the same time can strengthen or weaken the effect of the capecitabine tablets.
Be particularly careful if you are taking any medicines for:
- Gout (eg Allopurinol),
- Blood thinning medicines (eg warfarin),
- Some antiviral medicines,
- Medicines for seizures or tremors (eg pheytoin).
- Medicine that contains Folic Acid
Your hospital doctor or nurse must be made aware of these as they may advise you to stop the medication before you start your capecitabine or change the dose.
Your starting Capecitabine dose will be written in your printed copy of the leaflet. You will take them twice a day, and the chart looks like this in the leaflet.
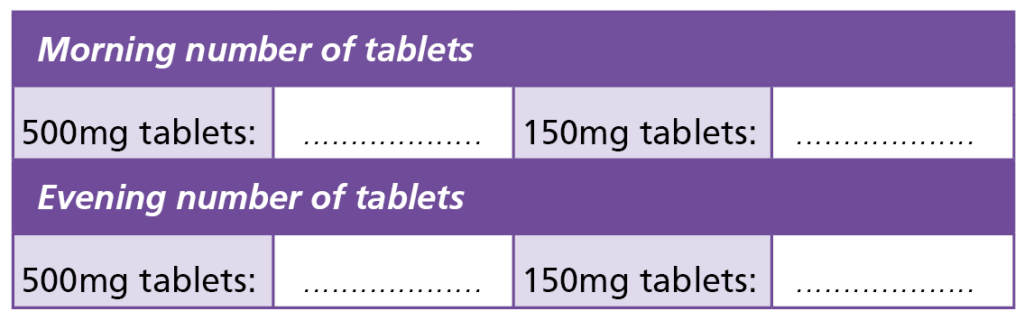
The dose may change over time so you might take a different combination of the two tablet sizes.
Blood tests
You will need to have blood tests before each supply of Capecitabine. These may be done at the hospital or at your GPs. If you live in Leeds the blood tests can be requested on the computer system but if you live further away you will need a blood card so the GP practice or local hospital knows what bloods to take.
What should I do if I experience side-effects?
If you experience any of the following side-effects on the next page or if you are feeling generally unwell or have any concerns please contact St. James’s University Hospital using the contact telephone numbers you have been given.
Important
Do not take any further capecitabine doses until it has been confirmed by your medical team that it is ok to do so.
If you are admitted to hospital please bring your Capecitabine tablets with you. You should let the medical team know that you are on chemotherapy tablets especially if you are admitted outside the oncology department. You should not take them until you have been reviewed by an oncology doctor.
Side-effects
| Diarrhoea | An increase of more than four bowel movements above your normal daily level or any at night. |
| Hand-foot syndrome or skin reaction | Angina-like pain in the chest. This may feel like a pain in the centre of your chest. If you experience this please ring 999 (Ambulance) immediately. Do not take any more Capecitabine tablets until you have been assessed by a Health Professional. |
| Vomiting (being sick) | If you vomit more than once in any 24-hour period. |
| Fever or infection | If you have a temperature of 38°C (100°F) or more, or show other signs of infection. |
| Nausea (feeling sick) | Feeling the need to be sick, this may give you a reduced appetite and you are finding it hard to eat and/or drink. |
| Chest Pain | Angina-like pain in the chest. This may feel like a pain in the centre of your chest. If you experience this please ring 999 (Ambulance) immediately. Do not take anymore Capecitabine tablets until you have been assessed by a Health Professional. |
| Mouth ulcers | If you have pain, redness, swelling or sores in your mouth, and you are finding it hard to eat and/or drink. |
Your treatment diary
How to use this diary
After you have taken each dose of Capecitabine, write down the time you take your tablets.
If you experience any of the side-effects mentioned, please make a note in the space provided even if they occur during your rest week.
If your doctor or nurse has told you to stop your dose of Capecitabine, write ‘stop’ until you are told to start taking it again.
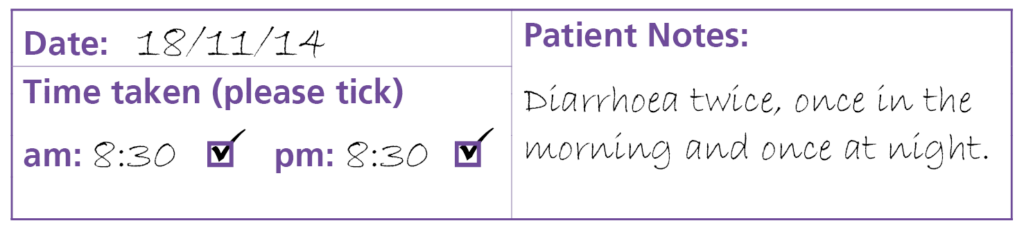
The diary section is not shown here but will be in the printed version you will be given when you start your treatment.
Local support services
Leeds Cancer Support
Leeds Cancer Support complements care provided by your clinical team. We offer access to information and a wide range of support, in a welcoming environment for you, your family and friends.
We can be found in the information lounges in Bexley Wing and also in the purpose-built Sir Robert Ogden Macmillan Centre.
The Sir Robert Ogden Macmillan Centre
The Centre is on the St James’s Hospital site and offers a variety of support services including complementary and supportive therapies. These therapies include Reiki, relaxation and visualisation, hand and foot massage and many others. We also offer a weekly exercise class and a monthly support group. You can just drop in for a coffee and a chat anytime.
Contact numbers for Leeds Cancer Support
Maggie’s Centre
If you or someone you love has cancer you may have lots of questions. Maggie’s is a warm, welcoming place where you can meet people who are experiencing similar things to you.
You may also be able to find support groups specific to your needs and get advice and information from their professional staff.
You don’t need an appointment and all support is free.