This leaflet aims to help you and your family understand more about your Distal Pancreatectomy (the removal of a part of your pancreas) to treat cancer, cysts and other conditions of the pancreas.
It will be given to you in addition to the information you will receive from your surgeon and their team.
We realise this may be an anxious time for you and your relatives. We hope that by providing accurate information you will know what to expect before and after your operation and feel better prepared.
This booklet will explain:
- What the pancreas does
- Why you need an operation
- What the operation involves
- Preparing for and recovering from the operation
- The potential risks of the operation
- Preparing to go home
St James’s University Hospital is a specialist regional centre for surgery on the pancreas.
You will be cared for by a healthcare team who are experienced in treating people having this type of operation.
On this page
- The Pancreas
- Distal Pancreatectomy
- Preparing for your operation
- Coming into hospital
- The day of your operation
- Recovering from the operation
- Potential risks and long term effects of surgery
- Long term effects
- The risks and benefits of the operation
- Going home
- Returning to normal
- Follow up
- Contact numbers
- Support Services
The Pancreas
The pancreas is part of the digestive system. It lies at the back of the upper abdomen in front of the spine and behind the stomach. It is about 20cm (eight inches) long. It has four sections: the head, neck, body and tail.
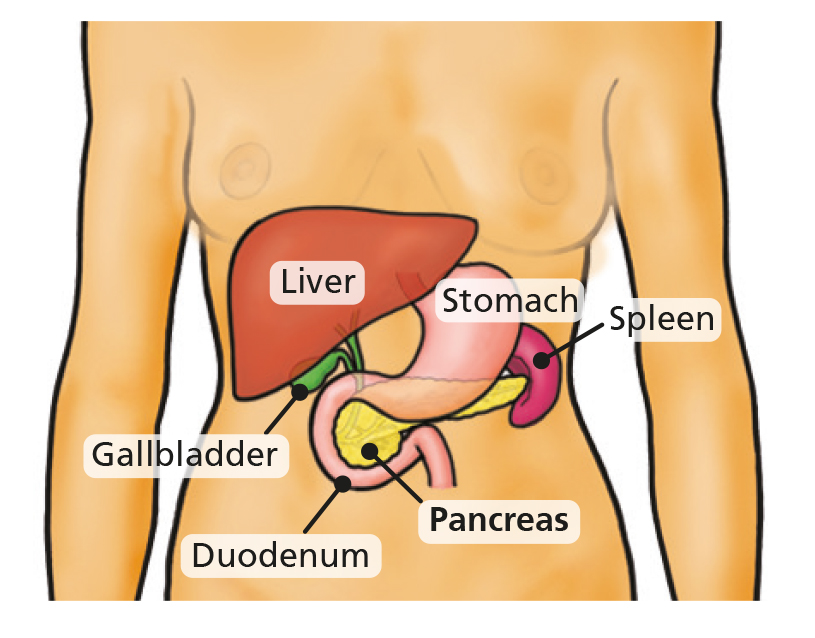
The pancreas produces:
- Pancreatic juice (enzymes) to help digest your food.
- Insulin to control blood sugar levels.
Distal Pancreatectomy
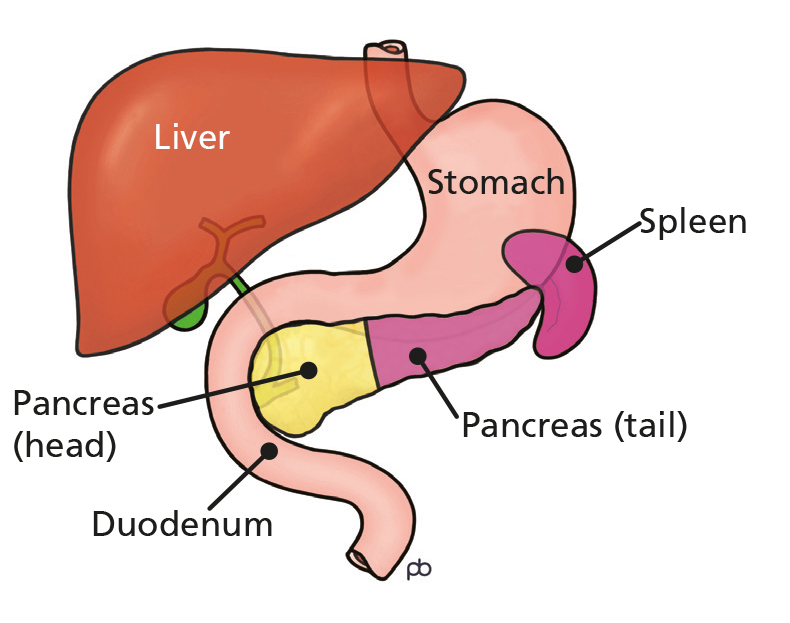
The surgeon removes the left half (body & tail) of the pancreas which is furthest away from the duodenum (first part of the small bowel), leaving the head intact. As the spleen is very close to the tail of the pancreas the spleen needs to be removed as well.
Pancreas before surgery
Pancreas after surgery
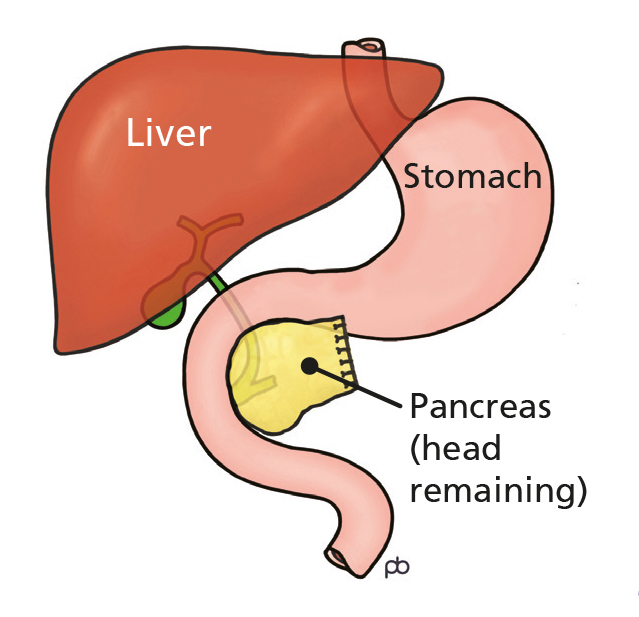
If your spleen is removed you will need lifelong antibiotics to prevent infections. Your surgeon will discuss this with you in more detail.
It is important to remember that very occasionally, at the time of your operation, surgery may be more difficult than previously thought. If this is the case your consultant may need to carry out more extensive surgery or may not be able to perform the operation.
Laparoscopic
Laparoscopic is a medical term for keyhole surgery. This is often the approach that is used. However, in some cases, your surgery may be more difficult than previously thought. If this is the case your consultant may need to carry out more extensive surgery or make a larger cut (open surgery), or may not be able to perform the operation. Your operation will be discussed with you after the surgery.
Preparing for your operation
Before your operation it is important that you stay as fit and well as you can. Taking regular exercise and eating nutritious food is very important. If this is difficult for you, please ask for advice from your doctor or specialist nurse. If you smoke, you should try to stop as soon as you can.
Stopping smoking, even just a few weeks before your operation, will make a big difference to your recovery and reduce your risk of developing complications.
Pre-assessment
To prepare for your surgery you will need some routine tests to make sure you are well enough for your operation. These tests are usually done in the pre-assessment clinic a few weeks before your operation.
You will receive an appointment to attend this clinic or you may have attended the clinic straight after your outpatient appointment. You will be involved in planning your care and recovery from the time you are seen in the pre-assessment clinic. This is a good time for you to tell us about your individual needs and circumstances. You will be asked about your general health, past operations, illnesses, allergies and medications you take. You may also have an ECG and blood tests.
This is a good time to start thinking about what support you may need when you go home after your operation. This is especially important if you live on your own. Are there friends, family or neighbours that may be able to help out with shopping, cleaning and cooking for a while until you are feeling stronger?
The nurses in pre-assessment will advise you about the trust’s infection prevention policy.
Coming into hospital
You will be admitted to hospital the day of your operation. A nurse and a doctor will talk to you and answer any queries you or your family may have. You will be given an identification band to wear on your wrist. If you have an allergy please let the staff know and you will be given an allergy band.
You will usually be visited by an anaesthetist who will explain about the general anaesthetic and how your pain will be controlled following your operation.
Medication
Most medication should be continued before your operation and throughout your hospital stay. Please bring your regular medication with you. However, some medication will need to be stopped before your surgery or a few days before your surgery to reduce any risks. This will depend on the medications that you are prescribed to take.
If you have a heart problem you must take your blood pressure medication. If you are taking a blood thinning medication e.g. aspirin, clopidogrel, warfarin you must inform pre-assessment and the surgical team. These medications may need to be stopped several days before your surgery.
Consent
A consent form is a document which we will ask you to sign to say that you agree to have the surgery. Your doctor will explain the details of your surgery to you and the risks associated with it.
Please do not be afraid to ask questions since it is important for you to fully understand the operation. If you have any questions about the operation it can be useful to write these down so you can remember the questions when you see the doctor.
The day of your operation
You will need to stop eating and drinking several hours before your operation. The nursing staff will advise you of the exact time (usually around midnight).
You will be given a hospital gown to put on. You will be asked to wear elasticated stockings as they help to prevent a deep vein thrombosis (blood clot) forming during the time you are less mobile. You will also be given a small daily injection to help thin your blood to reduce the chances of clots forming which needs to be continued for 28 days after your operation.
Recovering from the operation
You will be admitted to the pancreas ward, J82, in Bexley wing. On some occasions patients may require the High Dependency Unit (HDU). This will usually be for closer monitoring. While you are there your family will be able to visit. You will be awake and able to talk when you go to the ward or HDU but you may feel sleepy. You will be attached to various tubes and monitors, which the nurses will explain to you.
These may include the following:
Intravenous fluids (Drip): these are given through a tube inserted into a vein in your neck and/or arm to make sure you have enough fluid until you can drink again. Certain medications may given through this tube. Your consultant will decide when it is safe for you to begin to drink.
Naso-gastric (NG) tube: This is a thin tube that goes up your nose and down to your stomach. This will drain away any stomach contents to avoid sickness. This will be attached to a bag to allow it to drain freely and is usually placed when you’re having your surgery. The naso-gastric tube will usually be removed a couple of days after your operation.
Naso-jejunal (NJ) feeding tube: If your doctor thinks you need one, you may have a feeding tube. This tube goes up your nose and passes into your small bowel. This is used to give you liquid feed containing essential nutrients. It will stay in place until you are able to eat again.
Oxygen therapy: You will need oxygen for a number of days following surgery. Nursing and physiotherapy staff will advise you on some deep breathing exercises which will help to prevent you developing a chest infection. Deep breathing exercises are really important can help aid a speedier recovery.
A surgical drain: This is a thin plastic tube that may be inserted into your abdomen during your operation. It drains fluid away from the area of your operation. The removal of this drain will be graded by the samples the nurses take from the drain.
Catheter: During your operation a catheter will be inserted into your bladder. This is a tube which drains your urine into a bag, so we can measure how much urine you are passing. The catheter will stay in place until the surgical team advise forthis to be removed.
Once you are well enough you will be able to return to the ward.
Pain control
Your anaesthetist will speak to you before the operation about how to control your pain.
PCAS (patient controlled analgesia system): The most common form of painkiller is PCAS – a patient controlled analgesia pump. You will be given a handset with a button, which, when pressed, will give you a controlled dose of pain relief through a line in your arm. The pump has a security device which prevents you from taking too much medication.
Oral medication: Once the PCAS has been taken down you will be given regular pain killers, usually in the form of tablets. Our aim is for you to be as pain free as possible. If you experience pain please inform your nurse. The more comfortable you are, the more mobile you will be. The more mobile you are, the less likely you are to develop a chest infection or blood clot in your leg.
Wounds
Your wound will be checked regularly by the nurse for signs of healing and infection. A dressing will be applied where necessary.
If you have an open procedure then your stitches or staples are likely to be removed around 10-14 days after your operation. This may be whilst you are still in hospital or if you have gone home, by the practice nurse at your doctor’s surgery or district nurse. Sometimes we use dissolvable sutures, or glue, for the keyhole surgery that do not require removal and these will dissolve over time.
Personal care
After your operation you may need some help with washing and changing your clothes. You will be encouraged to take part in your care more as you feel stronger and have fewer tubes attached.
If you have any special needs or are worried about this aspect of your care please speak to your nurse.
Eating and drinking
You will be allowed to start eating and drinking a few days after your operation when the surgical team advise. This is to make sure the surgery inside your abdomen is allowed to heal. The nurses will help you to brush your teeth and tongue and use mouthwash to prevent your mouth and lips becoming dry and sore. You will firstly be allowed sips of water which will gradually be increased until you can drink freely. You will be given a light diet and encouraged to eat. The dietitian will see you whilst you are on the ward.
Once you are regaining your appetite and strength we welcome family to bring in food from home.
Please be mindful that we do not have the facilities to heat food up. However, we do have a patient fridge and we can label your food for you.
Potential risks and long term effects of surgery
As with all surgery, problems can happen during or after your operation. This can usually be dealt with by your doctor. The following information is specific to the type of surgery you are having.
It is important to remember that the majority of patients recover well from this major operation but complications can happen. Unfortunately some patients having this operation will experience a complication. Most of the complications can be dealt with easily. These include chest infection, wound infection or a urinary tract (waterworks) infection.
More serious complications include:
- Thrombosis in the legs or lungs
- Heart attack or stroke
The assessment you have before your operation helps us to identify patients who are more at risk of these complications. For all patients we have standard practices to reduce these risks. For those at increased risk you will be assessed by an anaesthetist and medications changed as necessary.
Serious complications can arise from the area of the operation and can include the following:
- Bleeding: Some bleeding is expected during your operation and occasionally a blood transfusion is needed. Bleeding can happen after surgery but this is rare. This can be managed either by the surgeon in theatre or by the radiologist in the x-ray department.
- Infection: Some patients may develop an infection such as wound, chest or urine infection. Infections can be treated promptly with antibiotics if necessary.
- Wound infection: Wound infections can be superficial (on the surface) or deep into the abdomen. The level of the wound infection will determine the treatment. Sometimes we may have to open the wound to allow the pus to drain out. In some cases a short course of antibiotics will suffice.
- Digestive juice leak: This can happen in the area where the pancreas should be divided/stapled and is a common complication of this surgery. If this happens the digestive fluid can leak out and make you unwell. If this happens it may delay your recovery and keep you in hospital for longer than expected. It is usually treated by draining the fluid. In a small number of cases may need further surgery or another drain inserted.
- Ileus: This is not uncommon following surgery and your bowel can go to sleep for a few days. Preventative measures are in place for this type of surgery for example, a nasogastric tube. However, sometimes the ileus may persist and you may experience nausea or being sick.
Long term effects
Diabetes
When part of the pancreas is removed the remaining pancreas may not be able to produce enough insulin to control your blood sugar levels. This puts you at an increased risk of developing diabetes because some of the insulin cells will have been removed.
Your blood sugar levels will be checked regularly while you are an inpatient. If your blood sugars remain high, this is a sign you may have developed diabetes.
This may happen a few months after your operation. If you feel thirsty or have excessive urine then please see your GP to investigate for diabetes.
If this problem does occur you will be given treatment, advice and support on how to manage this before you are discharged home. You should also speak to your GP about future monitoring of diabetes.
Pancreatic insufficiency
After surgery, some patients will not have enough pancreas remaining to produce the enzymes needed to digest your food. You may be given replacement pancreatic enzymes to take with your food. The doctors, nurses and dietitians will explain how to take these. Your consultant may start these enzymes before your operation. A dietitian may see you during your hospital stay.
Change in bowel habit
This operation may cause a change in your bowel habit. You may need to change your diet and eat smaller meals more often. The dietetic team will help support you with this.
The risks and benefits of the operation
There is a very small risk of dying from this operation. Around 1 in every 100 patients will die as a result of having this operation. This of course means that 99 out of every 100 people do not die.
Your consultant will discuss your own risk of having the surgery. It is important to remember that in general the surgery is performed for a diagnosis of cancer and therefore the risk of not having surgery has to be balanced against the risks of the operation itself.
Going home
It is important that you and your family, together with the nursing staff make plans for home as early as possible. This helps to make sure you do not have to stay in hospital longer than necessary. You and your family may have concerns about how you will manage and what to do if any problems arise. Please discuss any concerns you have with your doctors and nurses who will offer you help and advice.
You will need to continue with the ‘blood thinning’ injections for 28 days after your operation as you have received in hospital. If you are unable to do this please speak to the nursing staff so we can arrange for somebody to do these daily injections.
It is hoped that the following information will inform you of what you can expect when you go home.
Tiredness
By the time you go home you will be able to walk around your home and get yourself washed and dressed. You will feel tired however. Recovery from this operation is slow and may be 3-6 months before you feel back to your normal self. During this time you will gradually become stronger. If you live alone and are concerned about who will help you with shopping, cleaning and cooking etc, please speak to the ward staff who will discuss options with you.
It is important you take plenty of rest during the early days and weeks at home. You may feel you benefit from a sleep during the day. Increasing your level of activity as the weeks go by is important. Taking a short walk each day, increasing the distance gradually will have positive benefits.
Eating
By the time you are ready for home you will be eating and drinking again. Your appetite is likely to be greatly reduced and you may feel full very quickly. You will be advised to eat small meals and snacks often throughout the day rather than three large meals.
It is likely if you eat too much you may feel abdominal discomfort and bloating. You will soon learn how much food you can eat at any one time and you will adjust to smaller meals but more often during the day. Your doctor may have prescribed you medication to help absorb your food.
It is important that you take this medication just as you are about to eat your food. This will enable it to work more effectively. Most people do lose weight following this type of surgery, please be reassured that as your appetite improves your weight loss will stop and you will slowly start to gain weight.
Pain
Your wound may feel tender for a period of time after going home. Please make sure you take your painkillers as needed to keep you comfortable and be able to move around freely.
Bowels
Normally it takes a few weeks for your bowels to settle down into a regular pattern. Occasionally your painkillers may make you constipated. Please contact your GP or nurse specialist if you are concerned.
Returning to normal
It is understandable to want to know when you will feel back to normal after your operation. You may want to know when you can resume work, start driving or go on holiday. Although we know that recovery from this surgery takes several months, the rate of recovery is different from person to person and it is difficult to predict how long this will take in your case.
Follow up
Following your operation you will return regularly for check ups at the hospital. Your first clinic appointment will be approximately four weeks after going home. This will give you the opportunity to discuss any concerns or queries you may have. At the follow up appointment we will explain the pathology results found at the time of surgery and discuss the options for your next stage of treatment/after care.
Contact numbers
Support Services
Leeds Cancer Support
Leeds Cancer Support complements care provided by your clinical team. We offer access to information and a wide range of support, in a welcoming environment for you, your family and friends.
We can be found in the information lounges in Bexley Wing and also in the purpose built Sir Robert Ogden Macmillan Centre.
The Sir Robert Ogden Macmillan Centre
The Centre is on the St James’s Hospital site and offers a variety of support services including complementary and supportive therapies.
Please contact the centre 0113 206 6498 to find out what we currently offer.
Contact details for Leeds Cancer Support
Maggie’s Centre
If you or someone you love has cancer you may have lots of questions. Maggie’s is a warm, welcoming place where you can meet people who are experiencing similar things to you.
You may also be able to find support groups specific to your needs and get advice and information from their professional staff.
You don’t need an appointment and all support is free.