Your doctor has recommended that you have an ERCP. This leaflet will explain the procedure and what to expect on the day of your test. If you have any further questions, please telephone the department or discuss them with a member of staff on the day of your test.
What is an ERCP?
ERCP (Endoscopic Retrograde Cholangio Pancreatography) is a test to examine the bile duct or pancreatic duct. As a result of your previous tests, the doctors looking after you have asked us to look at your bile and / or pancreatic duct, and if we find a blockage, treat this.
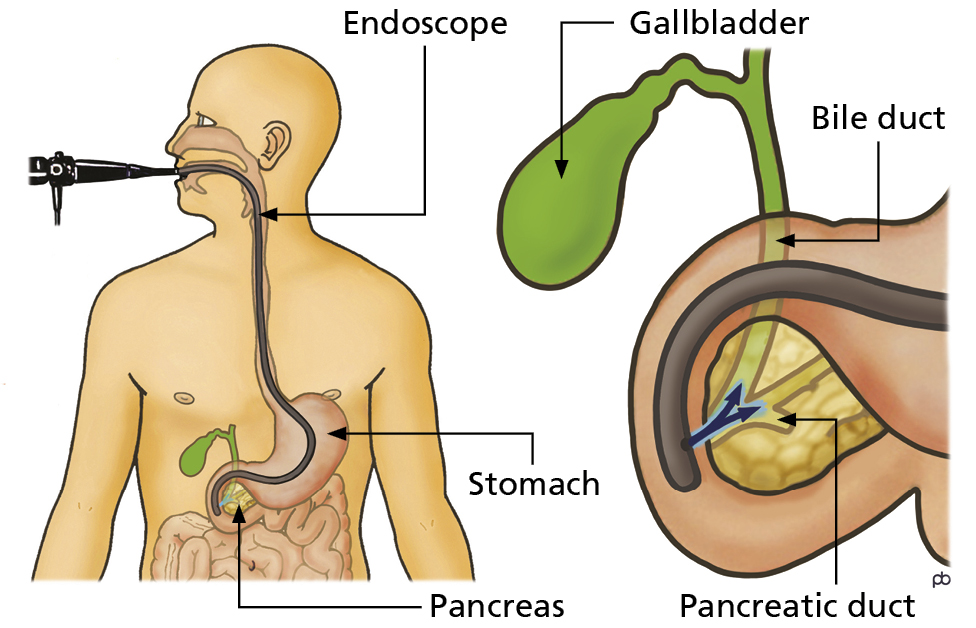
A flexible tube with a camera on the end is passed down your oesophagus (gullet) into your stomach and then into your duodenum (small intestine). The bile duct is then accessed by passing a small catheter through the camera. If a gallstone is found in the bile duct, the opening of the bile duct will be made bigger by cutting it open with an electrically heated wire; you will not be able to feel this. The stone can then be removed. Sometimes, stones are too big to be removed.
We have a number of other treatments that can be used in these cases. These will be discussed with you if your previous tests have shown that your gallstone may look too big to remove. If a blockage is found in the duct, we may insert a plastic or metal tube (stent) through the blockage to allow bile to drain. Stents may need changing after a few months if they become blocked.
What are the benefits / alternatives of having an ERCP?
An ERCP is an alternative to surgery and allows treatment, and detailed investigation of the bile duct and pancreatic duct. Any blockages and conditions such as gallstones can be treated immediately at the time of the ERCP without resorting to a full operation.
What are the risks and complications of an ERCP?
ERCP is a preferred procedure because it can provide a diagnosis and deliver treatment in a safer way than surgery; however, ERCP is not without risk.
The risk of a complication occurring is 5% – 10%. Most complications are mild and get better without needing an operation; however, some complications are more severe and require an extended stay in hospital, operations or admission to intensive care. This is very uncommon. Rarely complications can be life-threatening. The risks are detailed below:
Back to topWhat preparation will I need?
In order for good views of your stomach to be obtained, it is essential that the stomach is completely empty. You must not eat or drink anything for at least 6 hours before your test.
If you are an outpatient and coming directly to the Endoscopy Unit for your ERCP, your appointment letter will tell you when you need to stop eating and drinking.
If you are an inpatient on the ward, the nurses on the ward will tell you when to stop eating and drinking.
Do I keep taking my tablets?
You must keep taking any essential tablets unless your doctor tells you specifically not to. Please take your tablets early morning with a sip of water. If you have an afternoon appointment, please make sure you take your medication 4 hours before your appointment or leave it until after your test.
- Please telephone the Endoscopy Unit if you are diabetic, have sleep apnoea, have a pacemaker or are taking tablets that prevent blood clots. Examples of blood thinning tablets are Warfarin, Dabigatran, Apixaban, Rivaroxaban, Edoxaban, Aspirin, Clopidogrel (Plavix), Dipyridamole (Persantin), Prasugrel (Efient), Tigregralor (Brilligue) or Acenocoumarol (Sinthrome).
Will I be asleep for my ERCP?
ERCP is normally carried out under sedation. Sedation is not a general anaesthetic and will not put you to sleep; however, it may make you feel relaxed and forgetful. A painkiller Fentanyl injection is normally given along with your sedative Midazolam which will help you to feel more comfortable during the procedure. Local anaesthetic spray will also be given to numb the back of your throat.
What should I bring on the day?
Please bring a list of medication that you take and also any medication that you may require whilst in the department such as GTN spray, inhalers and insulin. Please do not bring valuables to the Endoscopy Unit or wear lots of jewellery. Please can you also ensure that you remove nail varnish as this interferes with the signal we receive from our monitors about your oxygen levels.
What will happen on the day of the test?
The ERCP will be carried out in the Endoscopy department. If you are coming as an outpatient, you will firstly be seen by a nurse. The nurse will ask you some questions about your medical history and your medication and any allergies that you have. The nurse will also record your blood pressure and heart rate. There may be a wait before you have your ERCP as we may need to confirm that a bed is available for you after the procedure.
The nursing staff will keep you informed about when a bed may be available for you if this is required. Before your procedure, the nurse will prick your finger and take a small sample of blood. This is to test the clotting factors in your blood. The nurse will also ask you to change into a hospital gown and insert a cannula (a thin plastic tube) into a vein in your arm or hand. The cannula will be used during the test to give you your sedation. If you are coming to the Endoscopy Unit from the ward, the nurses on the ward will prepare you for your procedure.
Before your test, you will be seen by the doctor who will be performing your ERCP. You will be given the opportunity to ask any questions that you may have about your procedure and also about your consent form before you sign it. By signing the consent form, you are agreeing to having an ERCP, that you understand why you are having the test and that the potential risks and complications of the test have been explained to you.
You will then be taken into an x-ray room where you will be greeted by two nurses who will remain with you during your procedure. The nurses and the endoscopist will complete a checklist to ensure all your information is correct. You will be asked to lie on your front on the x-ray table. You will be given oxygen through your nose throughout the procedure. A small probe will be placed on your finger to monitor your pulse and oxygen levels. A plastic guard will be placed gently between your teeth or gums. If you have any false teeth, you will be asked to remove these before the start of the procedure. Please let the nurse know if you have any loose teeth crowns or caps.
You will be given an injection into the cannula in your arm or hand to make you feel sleepy and relaxed. Once you are quite sleepy, a tube (endoscope) will be passed through your mouth into your stomach and then into the upper part of your small bowel (duodenum this is where the bile duct is situated). A fine plastic tube (cannula) is then inserted through the endoscope and into the opening of the bile duct. X-ray dye is then injected into the bile duct allowing x-ray pictures to be taken. During the procedure, you will be given a rectal suppository which contains medication that will help to reduce the risk of pancreatitis after your ERCP.
In a small number of patients, the sedation can cause them to become restless and quite uncooperative. In these cases, so the procedure can be completed, minimal restraint may be used (this usually means holding the patients arms). Incremental amounts of sedations may also be given during the procedure to ensure as much comfort as possible. If this is not possible or it is judged that it is unsafe by the doctor performing the examination, the procedure would be stopped. In this case, some restraint may be used until the procedure can be safely ended. On rare occasions, sedation given (either initial dosage or additional dosages), could impair breathing which could lead to low oxygen levels. If this were to happen, medications to reverse the effects of the sedation will be given.
Please note:
All hospitals in the trust are teaching hospitals and it may be that an endoscopist training how to perform an ERCP will complete your procedure under the direct supervision of a consultant.
What happens after the test?
After your test, you will be cared for by the nurses in the recovery room of the Endoscopy Unit. The nurse looking after you will monitor your blood pressure and pulse every 15 minutes until you are fully awake and recovered from your sedation. If you are staying in hospital, you will then be transferred to a ward. On the ward, your pulse and blood pressure will be monitored every 30 minutes for 2 hours, hourly for 2 hours and then 4 hourly. If your observations are satisfactory, you will be able to have a drink after 2 hours and a light diet after 6 hours.
Every effort is made ensure patients’ comfort during the procedure. In a proportion of patients, the procedure may be complex and lengthy, and it is acknowledged that there may be periods of discomfort during the procedure. This may impact upon your mental recovery, following the procedure. If you feel that you were affected mentally by any aspect of the procedure, please seek advice from your GP.
Most patients are seen as a day case and should be able go home on the day of their ERCP. You will be monitored in the Endoscopy Unit for 4 hours after your procedure and then reviewed before you are discharged home. If you have pain or signs of a complication, the doctor may recommend that you stay in hospital for the night for further observation.
Your letter will tell you if you are going home, or to a ward after your test.
Back to topRemember:
If you are going home, you will need an escort with you, transport home and someone to look after you for 24 hours after the test. You will not be able to have the procedure if this has not been arranged before the start of your test. If you are unable to make these arrangements, please contact the Endoscopy Unit.
You must not:
• Drive a vehicle
• Drink alcohol
• Operate machinery
• Sign legal documents
• Go to work
When will I get my results?
A full report will be sent to your referring doctor and your GP. The endoscopist or nursing staff will usually have the opportunity to speak to you after your test regarding the results.
This leaflet has been designed as a general guide to your test. If after reading this leaflet, you would like more information or are unhappy about having an ERCP performed, please speak to the consultant who has referred you for the test or contact the Endoscopy Unit on the numbers below.