Your doctor has recommended for you to undergo Image-Guided Liver Tumour Ablation. This leaflet will explain what the operation involves, the outcomes and the possible risks.
What is an image-guided liver tumour ablation?
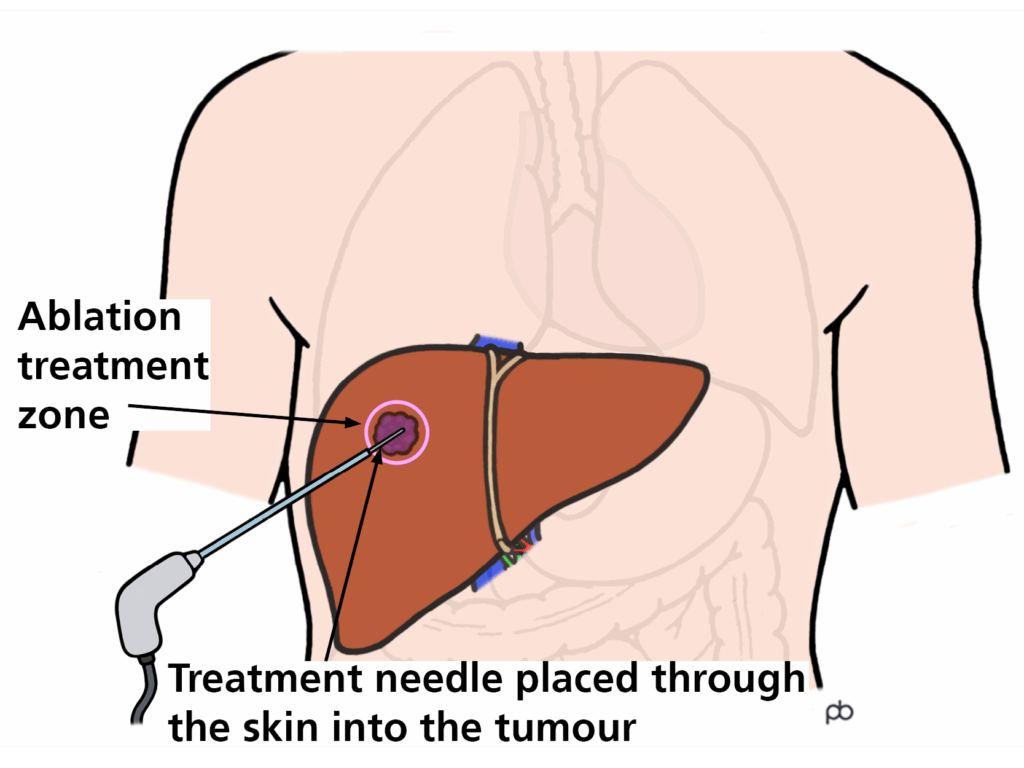
Image-guided ablation is a method of treating cancers within the liver without conventional surgery. It allows one or more cancers to be treated with minimal injury to the remainder of the liver.
How is an image-guided liver tumour ablation performed?
This operation is performed in the CT room under a general anaesthetic.
Using CT imaging, special needles are placed into the cancer. The number of needles required is determined by the size of the cancer.
Anaesthetic
This operation is carried out under a general anaesthetic. Your fitness for a general anaesthetic will be assessed in the Pre-assessment clinic.
Operation
Once you are asleep, the interventional radiologist will use CT imaging for guidance, will pass a special needle through a small puncture in the skin and position it within the cancer.
The needle is attached to a generator which delivers the energy to destroy the cancer. The energy used can be heat or electrical depending on the size and position of the cancer. The actual operation takes about 30-40 minutes but the whole operation might take 2-3 hours. This time may vary depending on how many needle placements are required.
Consent
You will meet the interventional radiologist in the interventional oncology clinic to discuss image-guided liver tumour ablation. The operating interventional radiologist will explain this to you in more detail, along with the risks and intended benefits before you provide your permission to proceed with the operation via a signed consent form.
What are the risks?
Serious complications are very uncommon. Everyone has their own risk factors that will be discussed during your first appointment. The pre-assessment anaesthetist will discuss with you the risks of having a general anaesthetic for this operation.
Common risks
- It is not unusual to develop flu-like symptoms known as “post-ablation syndrome” in the days following ablation which is related to the death of the cancer cells.
- There is a small risk of infection in the treated area; you will be given antibiotics if appropriate during the operation to try and prevent this.
- There is a small risk of bleeding. Very occasionally patients may need another procedure to stop the bleeding or a blood transfusion. If you take blood thinning medication, the nurse in pre assessment clinic will discuss with you if you need to stop taking them before your operation and from when.
- We are all exposed to low levels of natural radiation as part of our everyday lives and medical x-rays like CT scans give an extra dose of radiation. Radiation can increase your chances of developing a new cancer many years or decades after the exposure. The chances of this happening to you as a result of this procedure are about 0.3%, which is low compared to the natural risk of 50%. In some very rare situations, you may experience some reddening of your skin in the area that was treated. If this happens, please contact our team for clinical advice. It is important to remember that your doctor thinks that the benefits of this procedure outweigh any risks from the radiation, and we will make sure that the amount of radiation used in your operation is as low as possible.
Less common but serious risks
- In some patients, the lung or bowel may be close to the site of treatment, this risks damage to these structures. Occasionally additional manoeuvres at the time of ablation are required to push these structures away to try and prevent damage.
- Rarely more serious injuries or death may result from the treatment. The risk of such a complication is estimated to be about 1% or 1 in 100 treatments.
- Rarely, blood clots could form within the veins called ‘Deep Vein Thrombosis’, where you may need to be prescribed blood thinners for.
Are there alternative investigations / treatments?
The alternative treatments to ablation may include observation, surgery, focused radiotherapy, TACE, and chemotherapy.
There are many factors which favour different treatments including the number, size and position of cancers and your level of general fitness.
The risks and benefits of the different treatments would have been considered by your cancer specialist before referring you for ablation, but we can review these alternative options with you when you meet our team.
How well does it work?
In general, ablation is most likely to be successful if the cancers are smaller (<3cm) and limited in number (three or less).
Current guidance recommends either ablation or surgery for very early (1 < 2cm) or early (up to 3 with each <3cm) primary cancers in the liver. In very early-stage disease, 80-90% of patients are alive after five years; in early stage, 50-70% of patients are alive after five years.
In patients with a few (<3) small (<3cm) secondary cancers, ablation and surgery have similar outcomes. About 20-50% of these patients will be alive five years later.
What if the cancer grows back?
In a small number of cases about 5-10%, the cancer may not be successfully ablated. The treatment can be repeated, or your cancer specialist may suggest an alternative treatment.
Unfortunately, some patients will develop new cancers in their liver after treatment. If appropriate, ablation can be repeated.
What to expect from this operation?
Admission
You will be admitted the day before your operation onto the liver ward. On admission, you will have blood tests before your planned operation. On the day, the ablation team will consist of:
- Consultant Interventional Radiologist
- Clinical Nurse Specialist (CNS)
- CT radiographers
- Consultant Anaesthetist
- Anaesthetic Operating Department Practitioner
Pre-operative preparation
You will attend the pre assessment clinic for an anaesthetic assessment and investigations prior to the operation, which will include blood tests and ECG.
Pre assessment will take your medical history and review your medications. They will advise you if you need to omit any of your medication on the day or prior to the operation. If you are taking blood thinners, instructions to stop this medication may be given to you.
You will be assessed for Obstructive Sleep Apnoea (OSA). Sleep apnoea is when your breathing stops and starts when you sleep; this may require you to have further investigations. Please bring your CPAP machine on your admission if you normally use one at home.
You will be assessed for Methicillin-resistant Staphylococcus aureus (MRSA) and you will be given an anti-microbial body/hair wash and nasal cream. This will be discussed during pre-assessment, and you will receive instructions on how to use them.
Carbapenemase-Producing Enterobacterales, (CPE) are bacteria that usually live harmlessly in the gut of humans. You will be screened for this, which usually involves taking a rectal swab/stool sample.
You will receive a letter from the hospital with your admission date, ward, and instructions for fasting prior to the operation.
Recovery
After the operation, when you wake up you may have a sore throat. This is caused by the breathing tube placed in your throat while you were asleep.
You will be transferred to theatre recovery where you will be monitored. Once stable, you will be transferred to the ward.
Aftercare
Back on the ward, the nursing staff will continue to monitor you regularly. IV fluids and pain relief will be administered as prescribed by the doctor.
Blood tests will be performed the morning after your operation to review your full blood count and renal function. Most patients are discharged in the next few days.
Care at Home
We would advise that someone is at home with you the first night after discharge. After your operation, you may still experience pain or nausea, which can be managed by medications. Please see some of our recommendations below:
- Hydration: drink 2-3 litres of water a day. Adopt this as a lifelong habit as it helps to keep your kidneys healthy.
- Exercise: avoid lifting heavy items and other strenuous exercise for at least two weeks.
- Driving/travel: you should refrain from driving or flying until you feel well again, it is your responsibility to make sure you are fit to drive or fly.
- Medicines: you will be advised about restarting your medications before discharge. It is normal to experience mild pain and discomfort, continue your regular painkillers like paracetamol for the first week and reduce as pain decreases. If your pain persists and your painkillers are not working, please contact your GP to review your medications.
- Work: you should be able to return to work in 1-2 weeks, although some people may require a longer recovery period.
- Follow up: arrangements will be made for the Interventional Oncology CNS team to contact you after discharge via telephone to carry out remote follow up following your operation. Your liver team will arrange for you to have a CT or MRI scan performed 4- 6 weeks after your liver tumour ablation. Once this scan has been reported, the liver team will arrange an appointment to share the results of the scan with you.
Contact information
We hope some of your questions have been answered by this leaflet. If there are any questions you would like to ask before you come for your operation, please get in touch.