What is spasticity?
Spasticity can be described as involuntary muscle stiffness. It is a common symptom of neurological disease and can range from mild to severe and change over time, often from day to day or hour to hour. Other associated features can include spasms, pain, weakness and clonus (involuntary muscle contractions). Spasticity is not always detrimental, as some people use the stiffness in their muscles to help them stand, transfer or walk. However, prolonged spasticity may result in shortening of muscles, which further increases stiffness, limits range of movement of limbs and is not always responsive to drug treatments.
Why does spasticity occur?
Nerve pathways connecting the brain, spinal cord and muscles work together to co- ordinate movements of the body. These pathways can be disrupted in neurological conditions such as stroke, multiple sclerosis, cerebral palsy, head or spinal cord injury, leading to loss of this co-ordination and over activity of muscles causing spasticity.
How is spasticity managed?
Most people with mild to moderate spasticity can control their symptoms with exercises (including standing and stretches), physiotherapy, prevention of trigger factors and oral anti-spasticity medication. However despite appropriate treatment and management of trigger factors, spasticity can become severe and difficult to manage, affecting all aspects of daily life. Intrathecal Baclofen may be considered at this stage.
Trigger Factors for worsening spasticity
- Urinary retention or infections
- Bowel impaction, constipation
- Red or broken skin areas
- Poor positions in lying or sitting
- Tight fitting clothes or splints
- Pain
- Infections
- Low mood
What is Baclofen?
Baclofen is an anti-spasticity drug used to help control muscle stiffness and spasms. It acts by reducing the transfer of signals to and from specific nerve receptors found in the spinal cord and brain; this dampens down the effects of spasticity and associated symptoms. It is usually taken orally as a tablet.
Does oral anti-spasticity medication work for everyone?
No. Some people find that oral doses of anti-spasticity medication can help relieve their spasticity a little, but not totally or others find the side effects unacceptable. Common side effects from oral Baclofen can include weakness, drowsiness, fatigue and dizziness.
Why does Baclofen sometimes fail when taken orally as a tablet?
The brain has a protective mechanism known as the blood brain barrier, which prevents unwanted substances and sometimes drugs entering into the nervous system. When taken orally it is difficult for Baclofen to pass through the blood-brain barrier. This can result in too much Baclofen in the blood stream causing side effects (weakness, drowsiness and dizziness), and too little in the spinal cord to relieve spasticity.
What is ‘intrathecal’ Baclofen (ITB)?
‘Intrathecal’ refers to the space surrounding the spinal cord; this space is filled with cerebrospinal fluid (CSF). The CSF circulates around the brain and spinal cord acting as a shock absorber to protect these delicate structures. Baclofen medication is delivered to the intrathecal space using a programmable drug delivery pump. This is usually considered after all conservative measures have failed.
Why should Baclofen work when administered intrathecally?
Concentration of the nerve receptors sensitive to Baclofen are found in the spinal cord. Giving Baclofen intrathecally allows it to be delivered directly to the specific receptors. As the drug is being delivered directly onto the receptor sites, only small doses need to be used (about 1/100 of the oral dose). This can mean that the side effects such as drowsiness experienced with oral doses are less of a problem.
Does Baclofen work for everyone intrathecally?
No. Some people do not respond to Baclofen given intrathecally. A trial of the drug is necessary to see if a person responds to it.
What does the intrathecal Baclofen trial consist of?
- You will see the Neurosurgeon who will review you in clinic and arrange pre-operative assessment and plan the elective admission to a neurosurgical ward in Leeds General Infirmary to deliver this.
- Once admitted you will be seen by a doctor and measurements will be taken by the neurophysiotherapist including video recording of any specific goals highlighted by assessment (e.g. ease of positioning).
- Once you get to theatre, under general anaesthetic, Neurosurgeon will insert a lumbar catheter (thin tube in to your lower back) that will take about 30 minutes. Once you return to the ward, Baclofen will be administered via this catheter.
- Standard intrathecal Baclofen test dose is 25 micrograms as a bolus/single large dose.
- Physiotherapist will reassess 2-3 hours following the drug administration and take outcome measures and review the agreed goals.The side effects will be monitored too.
- If there is lack of beneficial effect the test dose will be repeated over next 2-3 days with a larger dose such as 50micrograms or 75 micrograms.
- The effect of the drug wears off in about 6 hours. Once the trial is complete the catheter is removed and you will be discharged.
- The outcome of the test dose is then discussed by the Multidisciplinary Team to decide if you would benefit with an intrathecal pump to deliver the drug continuously.
Responsive – what next?
If you respond to Baclofen and your goals are achievable, the nurse specialist will provide education and information on having a pump implanted that would provide you with
long-term treatment.
The consultant will be available to discuss all options. Following these discussions you may decide to have the pump implanted, which will be arranged by the Neurosurgeon.
What does a pump system consist of?
The pump system consists of a pump and catheter (Figure1). The reservoir in the pump, stores the Baclofen and the catheter connects the reservoir to CSF in the intrathecal space around the spinal cord (Figure 2). There are two pump sizes available: one has a 20ml the other a 40ml reservoir. We regularly use the 20ml pump; it is made of titanium and looks like a round metal disk 8.75cm (3.4 inches) in diameter. The pump is 1.95cm (0.77 inch) in depth and has an expected battery life of 5-7 years.
Figure 1
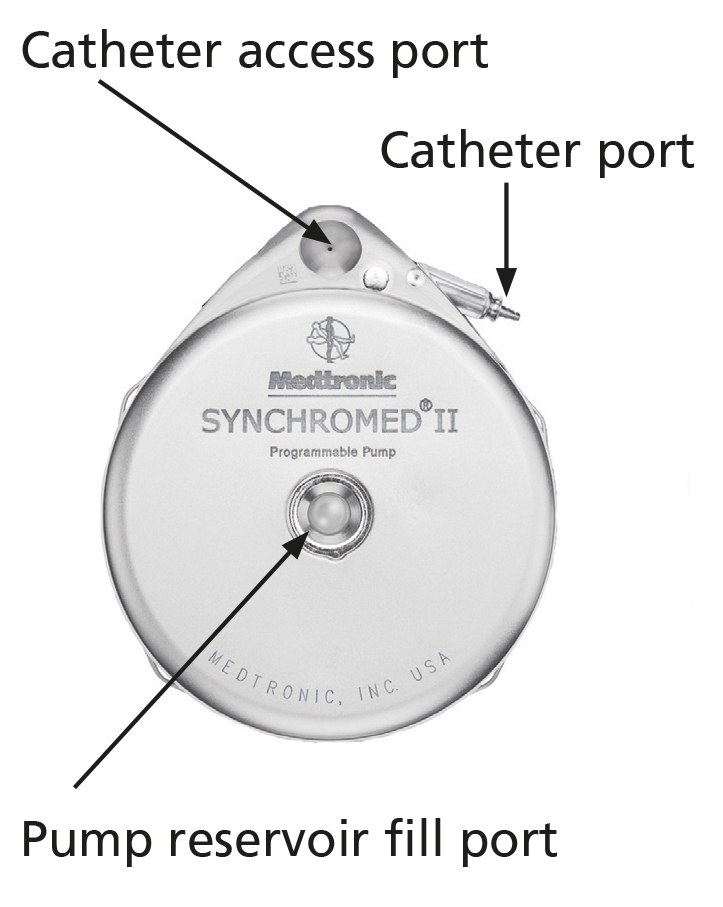
Reproduced with permission of Medtronic, Inc.
Figure 2
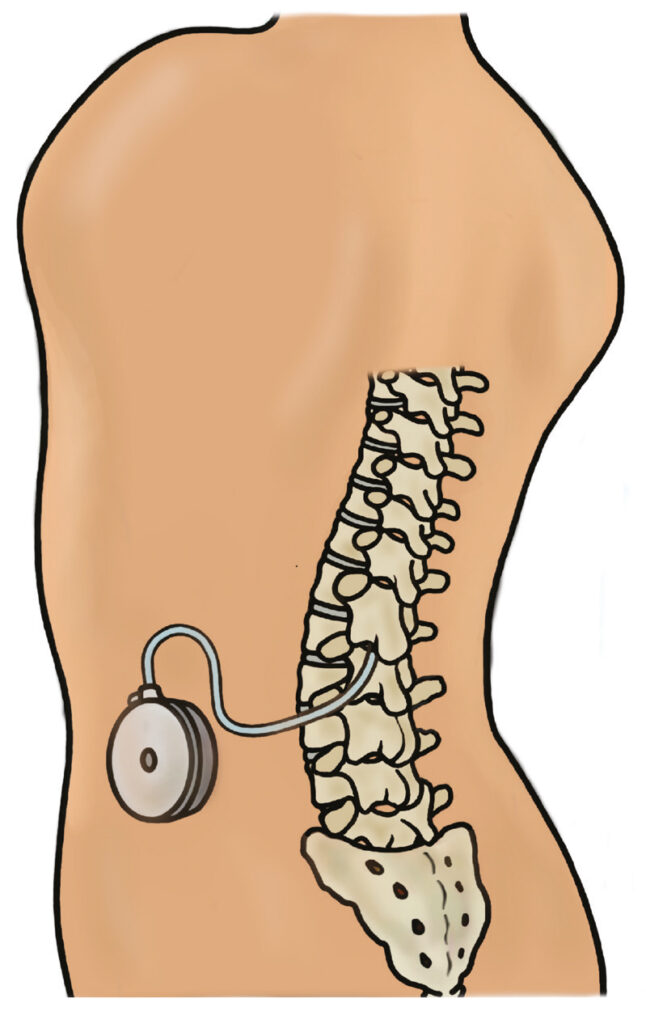
How is the pump implanted?
The pump is implanted under general anaesthetic by a Neurosurgeon in theatre. The pump is placed under the skin in the abdomen and a catheter connects this, with the fluid-filled space around the spinal cord so that the complete system remains hidden under the skin (See Figure 2).
The procedure, including being anaesthetised, the operation and time in the recovery room, can take approximately 2- 4 hours. The pump is filled with Baclofen in theatre and programmed to deliver an agreed prescribed dose in the recovery room. Once you are fully recovered from the anaesthetic you will return to the ward.
Programming the pump
- The pump has a microchip inside it which allows the amount of drug delivered to be programmed using ‘The Clinician Programmer’ (A tablet with an app). To programme the pump, ‘The Wireless communicator’ is placed lightly on the skin over the pump. (Figure 3)
- The pump has an alarm, which will sound if there is a problem. You will be told exactly what to do if this should ever happen
Does the pump work right away?
Yes. The pump will be programmed to deliver the intrathecal Baclofen at the prescribed rate as soon as you are awake following the surgery.
However it will take at least 4 hours for you to feel the full effect at that particular dose.
Figure 3 – The Clinician Programmer and the Wireless Communicator

Will the response be the same as the trial?
No. During the trial you will have received a relatively large, one-off dose of Baclofen to assess whether you respond to it. To administer it safely and effectively over time, much smaller amounts are required and are delivered continuously at an hourly rate. It may therefore be a few weeks before you feel the full benefit of the therapy.
Once the pump is in place the next step is to find the dose most suitable to you as an individual.
The aim is to find the dose that decreases spasticity enough to achieve your goals without causing unwanted side effects. This process takes time and involves gradually withdrawing any oral medication in use, so it is important to appreciate that it may take 2-3 months or longer to find the dose most suitable for you as an individual. It is therefore possible that your optimum dose will not be achieved before you leave hospital, as you may still be in the process of reducing oral medication and titrating the intrathecal dose up as an outpatient, while being assessed to achieve your set goals.
How long will I be in hospital?
Patients are generally discharged the following day after pump implantation. The stiches and/or clips in both your back (where the catheter was administered) and at the site where the pump was placed, if need to be removed should be after 10 days. One postoperative follow up in the Neurosurgical clinic will occur in 6-8 weeks to ensure the wounds have healed well.
How is the level of Baclofen in my pump reservoir monitored?
The nurse specialist will monitor the dates that your pump will require refilling and will liaise with you about when you need to attend an outpatient clinic. This can vary but is usually every 3-6 months for a refill.
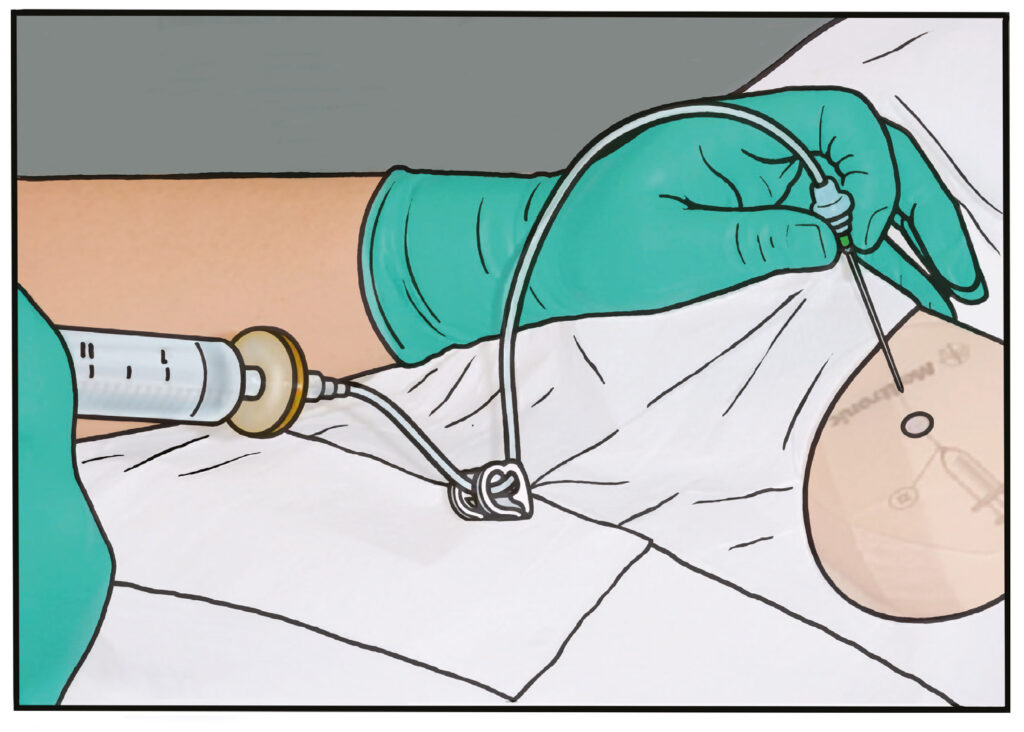
In the clinic, the nurse specialist and a doctor will review your current dose, assess how well your spasticity is being managed, and your pump will be refilled.
Refills involve placing a needle through the skin into the pump’s refill port and reservoir; this procedure may be uncomfortable but is not usually painful (Figure 4). The old Baclofen is withdrawn and fresh Baclofen is inserted. The pump is then programmed to deliver the prescribed drug dose.
Figure 4: Pump refill
Intrathecal Baclofen pump dosing and maintenance
The starting dose of the ITB pump will be determined by ITB team dependent on test dose and its response. There are different dosing modes for the Medtronic ITB pump (Continuous, Flex dose, Pulsed dose and Patient Therapy Manager (PTM)). The selection of the most appropriate dose and dosing mode will be decided by the ITB team on individual needs. The long term regular follow up will be by the Rehabilitation Medicine consultant to adjust the dose, dependent on selected goals and refills will be carried out by the nurse. Referral back to Neurosurgery is made when pump battery is depleted for replacement (usually in 5-7 years) and for any other surgical input when required. GPs will be kept informed of input provided.
What are my responsibilities?
- Contact the hospital if you feel there is a problem with the pump
- Know the signs of overdose and underdose (withdrawal)
- Know the correct contact procedure for non-urgent problems
- Know the emergency contact procedure
- Attend the outpatients department as scheduled for refills, clinical review of goals and dose
Frequently asked questions
In the past, people considering intrathecal Baclofen have asked us the following questions, which we have included here for your information.
Are there any risks from the surgery?
Yes, there are risks with any surgical procedure but we always try to minimise these. You will be seen by the surgeon and anaesthetist before your operation to go through any specific risks for you and to sign a consent form which will document risks.
During your operation we often take X-rays to confirm the position of the catheter and sometimes inject contrast or dye to help with this. The use of all ionising radiation is however kept to a minimum.
Blood clots are more common after surgery or bed rest. To prevent this, you may receive a blood thinning injection of Low Molecular Weight Heparin (LMWH) starting usually the day after your operation if required.
Infection is something we work hard to avoid so following your surgery we ask that you do not remove your dressings or get them wet until the stitches or clips are removed 7-10 days later. This means no baths or showers during this time.
Can the pump go wrong or stop working?
The main complication of the implantable pump system is that something goes wrong with the catheter; it is dislodged from the spine or becomes kinked or torn. If this happens a further operation is required to replace the catheter.
Studies have shown there is a risk of this occurring each year in the order of 5%, which means if we have 100 people with intrathecal Baclofen pumps, each year we would expect 5 of them to have a complication requiring an operation. Studies have shown that if something is going to go wrong with the catheter it is more common in the very early stages following implantation requiring a second trip to theatre during the initial admission. This however occurs in less than 10% (less than 1 in 10) of people.
The pump very rarely goes wrong or breaks down. If it stops working the main risk is Baclofen withdrawal. The nurse specialist will go through all the signs of this with you but the common effects are listed below. If you experience these you should contact the team for further advice. If the pump delivers too much Baclofen or there is a prescribing error you can present with signs of Baclofen overdose. This is an emergency and you will need to attend hospital to have the pump turned down.
Symptoms of Baclofen underdose/withdrawal
- Increase in stiffness or spasms, itching or goosebumps
- Fast heart rate
- Low blood pressure
- Fever
- Confusion, hallucinations, seizures
Symptoms of Baclofen Overdose
- Drowsiness
- Weakness of lower limbs
- Dizziness/Lightheadedness
Other side effects can include:
- Upperbody weakness
- Nausea/vomiting
- Low blood pressure
- Constipation or diarrhoea
- Slurred speech
- Weakness in arms
- Headache
- Numbness/itching/tingling
- Blurred or double vision
- Lethargy
- Difficulty breathing
- Seizures, difficulty passing urine
Oral doses of antispasticity drugs e.g. Baclofen and Tizanidine – do I keep taking them?
Yes. It is important that your oral anti-spasticity medications are slowly reduced under the guidance of the ITB team whilst in hospital and when followed up in the pump refill clinics. Sometimes if your arms have a lot of spasticity you may need to stay on an oral medication for spasticity long-term.
Will the pump cure my underlying condition?
No – it is important to appreciate that the pump is useful only in managing the symptoms of spasticity and spasms. It will not cure your neurological condition or influence its course.
Will the pump be visible?
Pumps are usually not visible under clothes. However, if you are very slim and wear tight clothing an outline of the pump may be seen. Before implantation of the pump you could be given an opportunity by the nurse specialist to wear a dummy pump taped to your skin. This will help you to decide the best position for the pump, taking into consideration the position of your waistbands and belts, comfort when sitting and lying and during sexual intercourse.
Can I wash and shower with a pump?
Yes – it is okay to wash and shower with a pump in place once the wounds have healed.
Can I have an MRI scan with the pump?
You can, but a nurse specialist will need to check the pump following the scan to ensure it has restarted as the motor may have stalled during this time.
Is it okay to have sex with a pump in place?
Yes – some people have expressed concern that the pump may be displaced or damaged during sexual intercourse. The pump is placed in a deep pocket in the abdomen, so it is well protected.
What about pregnancy?
If you are pregnant or would like to become pregnant it is really important to tell your doctor straight away. Sometimes we will advise to reduce your oral medication but you should never stop medication suddenly. Having an intrathecal pump in place is quite safe for a baby as only a very small amount of Baclofen is infused and hardly any will be in the bloodstream, in fact much less than if you are taking tablets. The ITB team will liaise with your obstetric team about delivery especially if you will be having an epidural or caesarean section. If you are likely to become pregnant in the future we will discuss with you any special considerations like the position of the pump or length of the catheter with you before your surgery.
Will I be able to travel abroad with a pump?
Yes – it may be possible for the nurse specialist to liaise with the pump manufacturer (Medtronic) to help identify contact names and numbers in case of an emergency when travelling abroad. You must check before travelling abroad that you have enough Baclofen in the pump to cover your time away. Before discharge, the nurse specialist will give you an identification card that will detail the type of pump and drug you have along with our contact details – it is advisable to carry this with you at all times in case of emergency. Note that your pump may set off the metal detector at airports, so please present your identification card to the security personnel.
We advise that you take oral Baclofen if required when abroad.
How long does the pump last?
The battery that powers the pump lasts approximately 5-7 years. Each time we refill your pump we get an estimate of battery life remaining. A planned admission will be arranged for replacement of the pump before this time.
The replacement involves removing the pump from the abdomen and attaching a new pump to the existing catheter; this is again performed under general anaesthetic.
Is it possible to be cremated with a pump?
Some people have expressed concern about this issue. If you plan to be cremated please note that the pump needs to be removed by the funeral directors prior to the cremation.
The removal of medical devices is regular practice for undertakers so they will be used to doing this.
Can I take other medications?
If your doctor is prescribing any medication they will avoid any medication that cannot be used in combination with Baclofen.
Will the pump interfere with my daily activities?
The presence of the pump should not curtail your lifestyle. Overall, you may find that the pump increases your ability to participate in daily activities.
For many people, a reduction in stiffness and spasm leads to an improved quality of life.
Is there anything I should avoid doing once the pump is in place?
We would recommend avoiding extremes of movement to the spine, including stretching backwards (for example adopting the yoga ‘cobra’ position) and curling up (for example holding both knees to your chest or reaching down to touch your toes). Stretches to the lower back in which you lie with your knees bent and then rotate your legs to the side into a corkscrew position are also best avoided. This is because it is possible that, during extremes of spinal movement, the intrathecal Baclofen system can become overstretched and potentially damaged.
Prolonged direct pressure over the pump and catheter (for example lying on your tummy or wearing tight fitting clothing), should also be avoided. Please ask your therapy team to review any wheelchair lap-straps, hoist slings and transfer aids to ensure they are compatible with the intrathecal Baclofen system. Power plates (Vibrogym) should not be used and please seek further advice from the team if you scuba dive or go for hyperbaric oxygen therapy.
Please check the patient manual from Medtronic, as this highlights all other activities that require caution or should be avoided. Contact the team if you need any further guidance.
What support is available when I am at home?
Your GP will receive information on intrathecal Baclofen and the contact procedures. If other health care members are involved in your daily life, copies of information packs can be made available to them on request.
The nurse specialist is available to offer advice and education to your community and social care team as needed. The nurse specialist is available Monday to Friday at below hours.
If it is a 6 week post-operative period with a pump related issue: Call the Neurosurgery wards L24/L25 for advice (see page 23) or attend A&E in an emergency.
Out of Hours: Most symptoms are not related to the pump system or the Baclofen drug. So a clinical review by a GP/A&E need to rule out other medical/surgical cause for presentation.
Commonly worsened spasticity, spasms could be related to a new onset infection (most commonly urinary tract infection), bowel/bladder problems, (constipation, renal stones, urine retention) fracture or joint problems, pain, skin/soft tissue problems (e.g: pressure ulcer, ingrown toenail) etc. which will need to be addressed to relieve symptoms.
Your GP or A&E doctor may contact Neurology/Neurorehabilitation /Neurosurgery on call doctor to get advice on temporary management of symptoms pending a review by the ITB team on the next working day if it is suspected to be due to a pump related issue.
If your questions have not been answered here, or if you wish to discuss any aspects further, please don’t hesitate to contact.