This leaflet has been produced to advise you and your parents and carers how to keep your skin healthy whilst in hospital, some information will also be helpful when you are discharged home.

- Surface
- Skin Inspection
- Keep Moving
- Incontinence
- Nutrition & Hydration
What is a pressure ulcer?
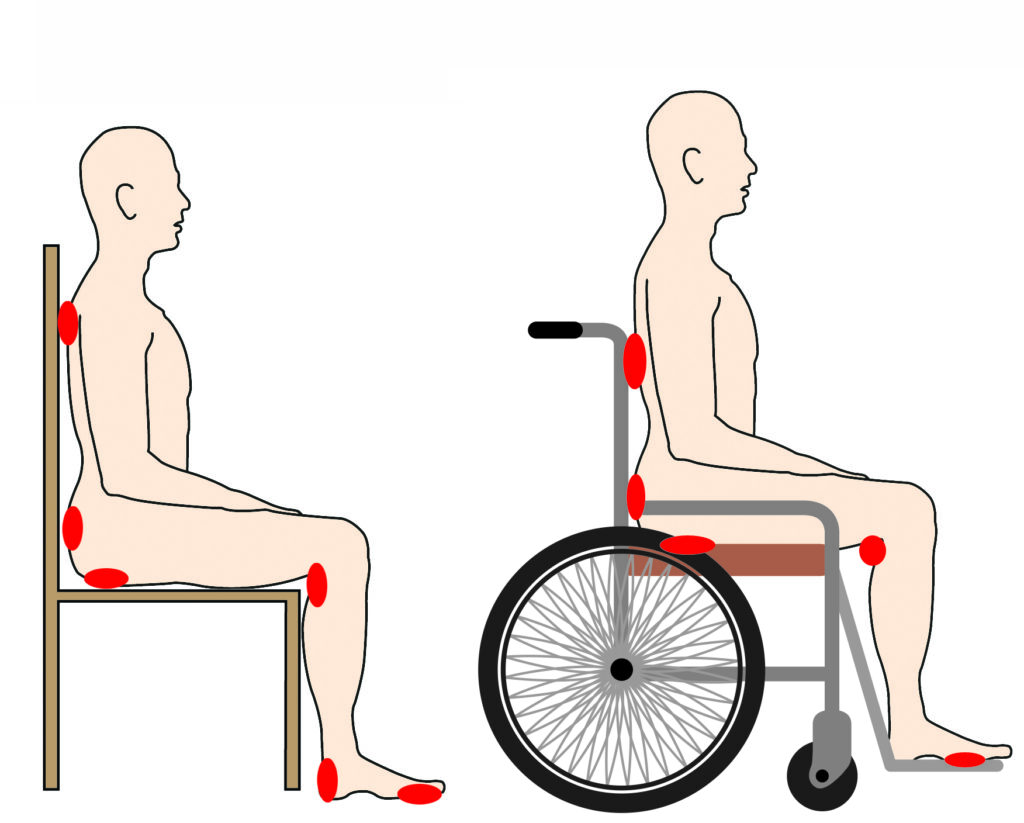
Pressure ulcers, also called bed sores, are parts of your skin that become damaged and sore. They happen when you are sitting or lying in one position for too long. They can also be caused by shoes that don’t fit properly, sliding down the bed, wheelchairs and chairs that don’t fit you and not being able to keep your skin clean and dry.
Who may get pressure ulcers?
Some people are always at risk of pressure ulcers. Everyone’s at some risk in hospital because you don’t move around as much as usual. This may be because you’re tired, taking medicines or are in pain. You are more at risk if you are:
- Having strong pain killers such as morphine.
- Not eating and drinking enough.
- Overweight or underweight.
- Stay in the same position for long periods (bed or chair).
- Your skin may be – dry, moist, red, sore or swollen.
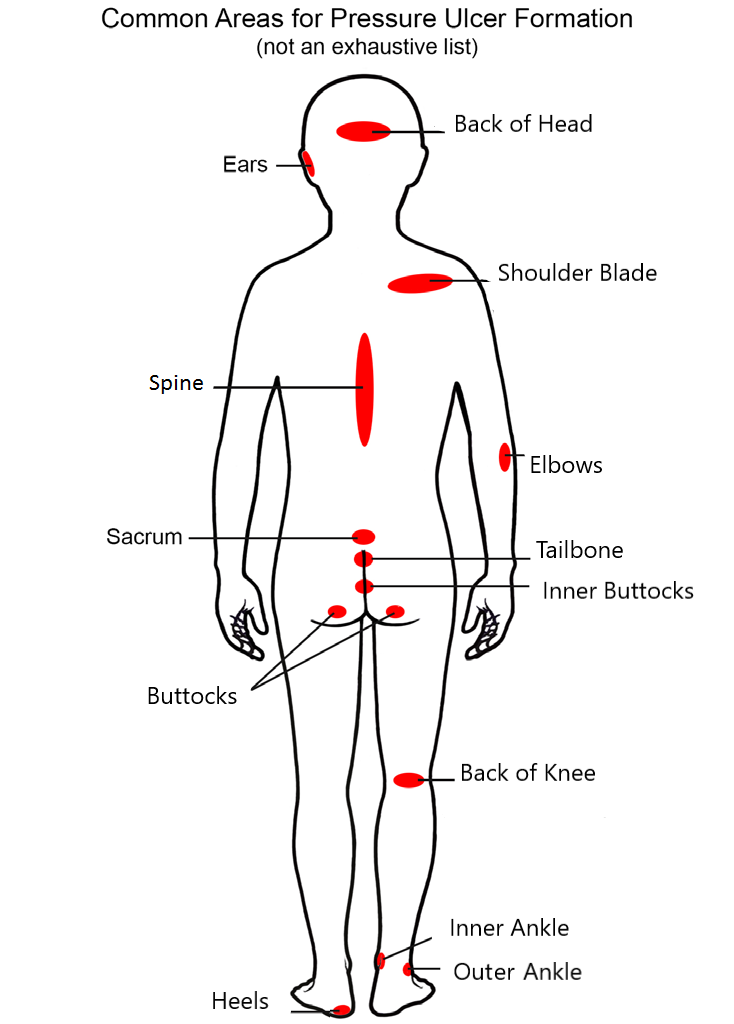
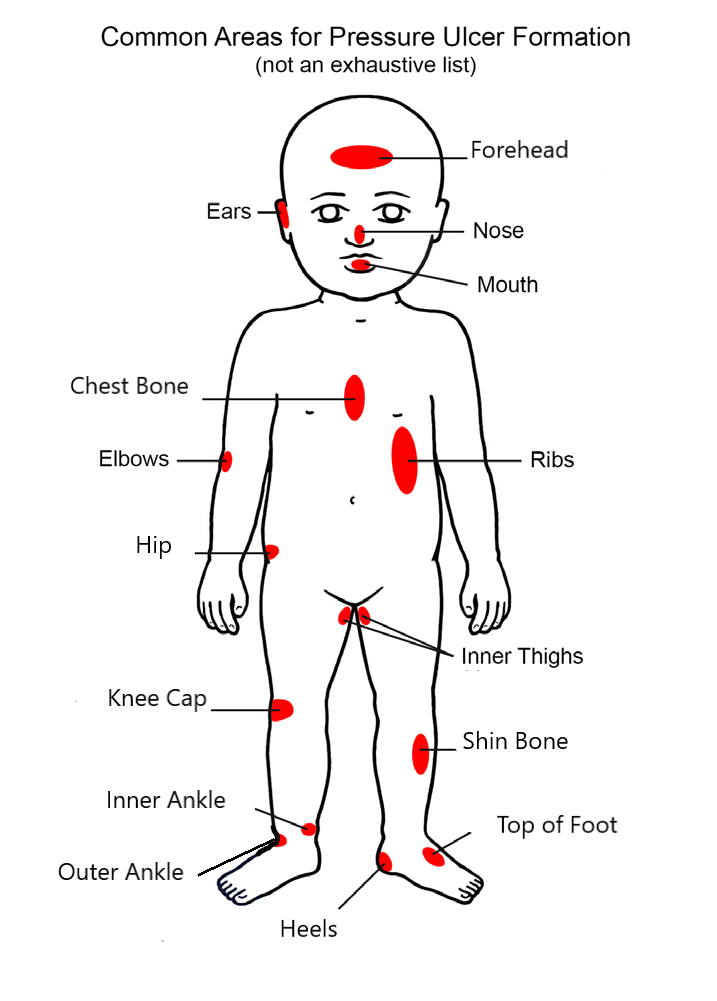
Checking your skin – get to know your pressure areas

The red dots are parts of the body where pressure ulcers are most likely to happen. These may start off as red marks.
Surface

We can help by giving you special mattress or cushion if you are at risk. Please tell the nurses if the equipment you have been given is not working or is uncomfortable.
Please tell nursing staff if you normally
use a special cushion or mattress at home. Pressure ulcers can also happen under medical devices. Such as oxygen masks, cannulas, urinary catheters, casts, or neck collars.
It is important that you tell the nursing staff if any of these are painful, rubbing against the skin or poorly fitting.
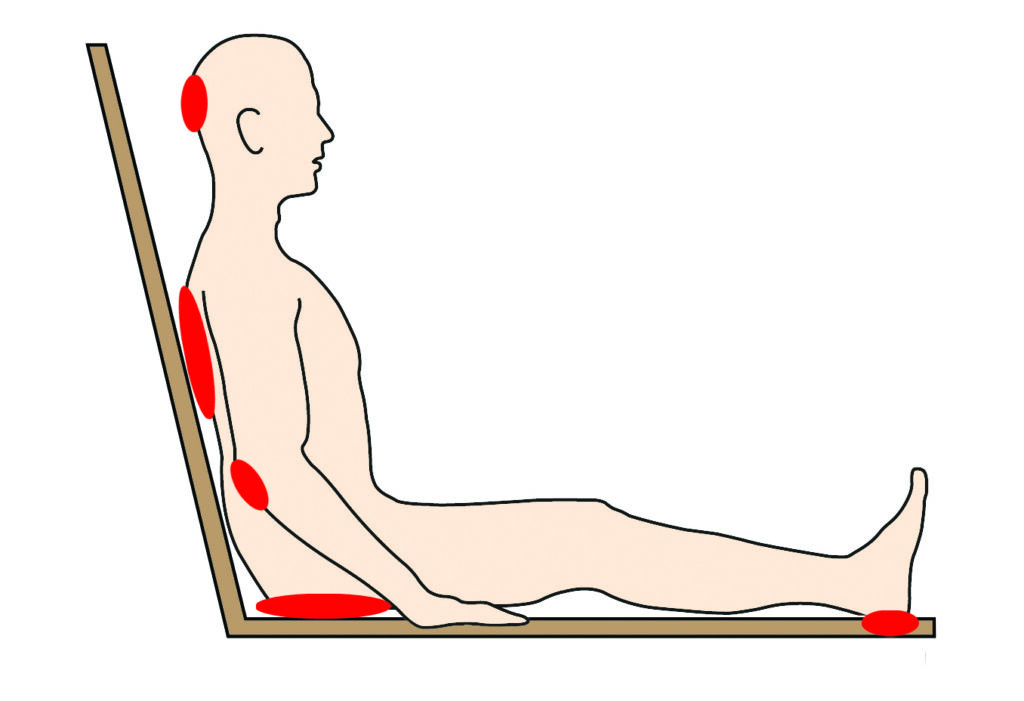
Keep moving
It might be that you are more at risk of a pressure ulcer because you are not able to move around as much as usual.
Moving around regularly is very important to help prevent a pressure ulcer. You can keep moving even if you are sitting or lying in bed or in a chair.
We have staff in the hospital who can show you how to do this.
Moving side to side and lifting your bottom helps makes the pressure easier for a short time.




Use your call bell to ask the nurse if you need help with this.
(Images used with kind permission of Catherine Cross – Physiotherapist.)
Moisture
Your skin can get wet and damp from your wee, poo or if you get sweaty.
If your skin is wet or damp it can get sore if it rubs on sheets or if you are sitting still for a long time.
We will keep your skin clean, dry and moisturised. The nurses will check your skin every day. It is good to keep yourself clean, please ask the nurses for help and advice.
A foam cleanser can help to keep skin clean and a barrier product protects your skin. Make sure your skin is patted dry not rubbed after washing and use moisturisers. You can speak to your nurse for more information about these products.
Patient quote:
I’m glad I told the nurses that my bottom was sore, because we caught the ulcer early.
Eating and drinking
If you are not able to eat and drink as much as you do usually, your skin may not be as healthy as normal. If your skin is not healthy it can get sore more easily.
Drink plenty of fluids (unless we have told you not to) to help keep your skin healthy. This can be water, juice, squash or milky drinks.
Losing weight because you are not eating properly can make it easier for your skin to become sore. If you are overweight or underweight it can also cause problems for your skin.
The nurses will check how much you weigh when you first come into hospital and every week. If they have any worries, a Dietitian (someone who is a food expert) may come to see you. They will give you help and advice about the food you.
Remember, it’s important to look after your skin by:
- Moving regularly.
- Eating and drinking well.
- Telling staff if you have any pain or discomfort.
If you would like any more information or have any questions, please speak to a staff member on the ward or ask your mum, dad or carer to speak to them.
Staff are able to ask other members of the hospital team to see you. This may be the Tissue Viability Service, Physiotherapists, Dietitians and Occupational Therapists. They are there if you need special help or if you are still feeling poorly.
Also available in easy read format.