You have been referred for an operation for an abnormality within or near the pituitary gland.
We find that most patients have similar concerns and this patient information handbook is intended to explain some of the surgical aspects of your treatment and hopefully to put your mind at ease.
On this page
- Leeds Pituitary Centre Team Introduction
- Leeds Pituitary Centre – Introducing the Team
- Leeds Pituitary Team
- Pituitary Gland
- Signs and Symptoms of a Pituitary Tumour
- Diagnosing Pituitary Tumours
- Treatment of Pituitary Tumours
- Decision to perform surgery
- Pituitary – Decision to undergo surgery
- Surgery
- On the day of surgery
- Pituitary – On the day of surgery
- After your surgery
- Pituitary – After surgery
- After discharge home
- Pituitary – After discharge home
- Post Operative Instructions
- NeilMed Sinus Rinse
- Follow up after the surgery
- Pituitary – Follow up
Leeds Pituitary Centre Team Introduction
Leeds Pituitary Centre – Introducing the Team
Hello my name is Rosen Daly and I’m the specialist nurse for pituitary anterior skill-based surgery.
In this video we’d like to introduce the team who will be involved in your care at the leads pituitary Center the team is made up of neurosurgeons ENT surgeons endocrinologists Radiologists specialist nurses as well as has the invaluable support of Junior doctors nurses and Allied health professionals surgery at Leeds.
Is performed with the expertise of a neurosurgeon and ENT surgeon our neurosurgeons are Mr Phillips, Mr Tagi and Mr Shake and our ENT surgeons are Mr Nicks Mr Simes and Mr Wilson all of whom have a specialist interest in endoscopic pituitary surgery.
Our pituitary endocrinologists are Dr Murray, Dr kakis and Dr Sejour in addition to the oversite of our endocrinologists you may have follow up under care of an endocrinologist.
In your local hospital our oncologist is Dr flattley. My role as nurse specialist for pituitary and skull-based tumor surgery is to offer support and information and to prepare you for your surgery and Recovery.
I can offer an holistic needs assessment and if there’s anything that is important to you that you wish us to know about please do contact me further to discuss in addition to myself we also have a specialist nurse in endocrinology Mel Gerard who is your point of contact regarding the endocrinological aspects around your operation.
Leeds Pituitary Team
You have been referred for an operation for an abnormality within or near the pituitary gland. We find that most patients have similar concerns and this patient information handbook is intended to explain some of the surgical aspects of your treatment and hopefully to put your mind at ease.
There are also some useful contact details for further information and advice in this leaflet. Your surgical and endocrine team will be happy to explain any further queries and unfamiliar terminology.
The Leeds Pituitary surgical service serves a population of about 2.5 million people centred on West Yorkshire and beyond. Pituitary surgery is undertaken in adults and children at the Leeds General Infirmary.
We also accept and treat patients referred from outside the region, including overseas patients. New patient referrals from within the UK require a referral letter from a patient’s General Practitioner.
Pituitary surgery in Leeds is mainly done through the nose, with the expertise of neurosurgeons and ear, nose & throat (ENT) surgeons.
| Neurosurgery Consultants | Pituitary Endocrinologists |
| Mr Nick Phillips Mr Atul Tyagi Mr Asim Sheikh | Dr Robert Murray Dr Nikolaos Kyriakakis Dr Khyatisha Seejore |
| ENT Consultants | Oncologist |
| Mr Paul Nix Mr Tom Wilson Mr Panas Symeonides | Dr Michael Flatley |
| CNS team | |
| Pituitary Surgery Roisin Darley | Leeds Endocrine Mel Gerrard |
As part of a multi-disciplinary team (MDT), the pituitary surgeons work closely with Endocrinologists across the Yorkshire region, Neuroradiologists, Oncologists, Pathologists,
Neuro-Ophthalmologists and Specialist Nurses.
Pituitary Gland
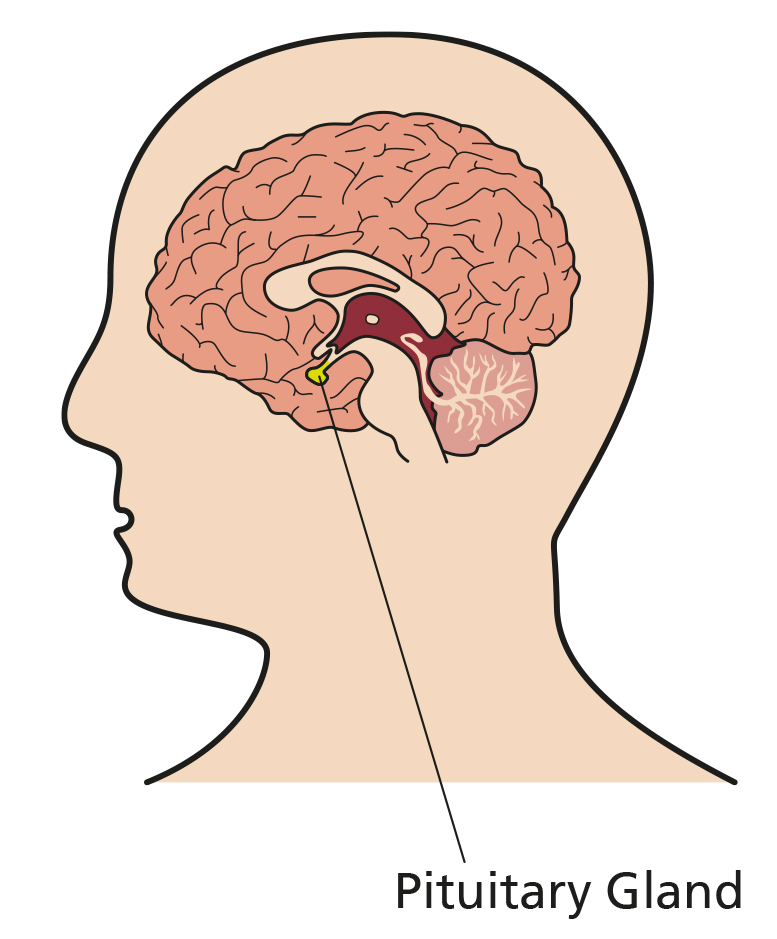
The pituitary gland is a small gland that sits inside a bony cavity in the midline, between and behind both eyes. The normal gland is about the size of pea and secretes hormones directly into the blood stream. The pituitary gland is responsible for producing hormones that regulate various organs and glands in the body, including the thyroid gland, the adrenal glands, the ovaries and the testicles.
The pituitary gland regulates a number of the body’s hormones and which in turn play a role in maintenance of multiple bodily systems. These include growth during childhood, fertility, weight, salt and water balance, the menstrual cycle, sexual function, energy levels and well-being.
A pituitary tumour, is an abnormal growth in the pituitary gland. Up to 20% of people have small pituitary tumours or cysts, most of which remain undiagnosed as they rarely cause any problems. Most pituitary tumours are non-cancerous (benign). “Functioning” tumours produce hormones. They cause symptoms accordingly, depending on the hormone being produced. Those that do not produce hormones are called “Non-Functioning” tumours.
Signs and Symptoms of a Pituitary Tumour
Pituitary tumours can cause symptoms due to the tumour pressing on surrounding structures, failure of the normal pituitary hormones (Hypopituitarism), or the pituitary tumour producing an excess of a hormone (Functional pituitary tumours). For example,
1) Pressure Symptoms
Loss of peripheral vision, headaches, watery discharge from the nose (cerebrospinal fluid leak)
2) Hypopituitarism
Weight gain or loss, lethargy, dizziness, nausea, vomiting, loose stools, dry skin and hair, thin bones, infrequent or absent menstrual cycle, loss of libido, erectile dysfunction, hot flushes, mood changes.
3) Functional Tumours
- Growth hormone secreting tumours (Acromegaly) can lead to large hands and feet, a change in facial features, excessive sweating, headaches
- Prolactin secreting tumours (Prolactinoma) often lead to breast milk discharge (galactorrhoea), infrequent or absent menstrual cycle, loss of libido, erectile dysfunction, hot flushes, mood changes
- ACTH secreting tumours (Cushing’s syndrome) lead to an excess of the natural steroid, cortisol. This often presents with flushing and roundness of the face, purple stretch marks, easy bruising, weight gain, muscle weakness, thin bones and menstrual irregularity
- TSH-secreting tumours lead to an overactive thyroid gland with weight loss, palpitations, shakiness, heat intolerance and sweating
Rarely pituitary tumours present with pituitary apoplexy. This is a syndrome resulting from a spontaneous stroke or bleed in a pituitary tumour and causes some combination of: acute severe headache, visual impairment, double vision, drowsiness, confusion or low blood pressure. This is a medical emergency and warrants immediate presentation to your nearest emergency department.
Diagnosing Pituitary Tumours
The suspicion of a pituitary tumour is raised either by presenting symptoms (as above), abnormal hormone levels, or not infrequently is discovered when head imaging is performed for an unrelated reason. Further investigation usually includes:
- Blood tests to check hormone levels released from the pituitary gland
- Goldmann visual fields
- Dedicated MRI scan of the pituitary
- Further specific tests are required where a functioning tumour is suspected
Treatment of Pituitary Tumours
Treatment of pituitary tumours may involve surgery, radiotherapy, medical therapy (some functioning tumours), or a combination of these treatments.
Most large tumours of pituitary gland will require removal via surgery. Tumours that produce Prolactin can generally be treated with medicines. Sometimes, if there is tumour residuum or recurrence, other medication, further surgery or radiotherapy may be advised.
Prior to and after surgery we may ask you to fill out a questionnaire or two on your symptoms. This helps us to understand the impact of the diagnosis and treatment on you and allows us to improve our services. We would be grateful for your participation.
We sometimes use radiological images and operative videos for teaching purposes and publication on social media and medical journals. These are used as anonymous pictures with no identifiable data. This will usually be discussed with you at the time of consultation in clinic. If you do not wish the images to be used for teaching purpose, please indicate this at the time of consultation.
Decision to perform surgery
Pituitary – Decision to undergo surgery
I would like to elaborate on what to expect once the decision to proceed with surgery has been made in clinic with your neurosurgeon whilst awaiting a date for surgery.
You will be booked into a pre-assessment clinic this is usually a nurse-led clinic where you will have pre-operative blood tests routine swab tests and an assessment made regarding any other medical conditions you may have and that may impact on the safety of surgery.
Should you have any other serious medical conditions a consultant anesthetist may be involved in this assessment and additional tests may be requested.
I will also be in contact with you before the operation to speak with you about what to expect and to answer any specific questions you may have our patient information leaflet should be able to answer the most frequently asked questions.
You may have you may receive some pre-operative questionnaires and we would be grateful if you could complete these once the date the surgery is scheduled you should be informed about any medication that you should stop prior to surgery for example any blood thinning medication like aspirin or clopidogrel or warfarin.
You will also be given instructions about fasting prior to surgery this is usually not having anything to eat for at least six hours before surgery and only clear fluids up to two hours before surgery.
Surgery
Surgery to remove a pituitary tumour is needed if the tumour is pressing on the nerves to the eyes, and as the first treatment for some functional tumours, this is called endoscopic trans-sphenoidal surgery.
Most of the time, pituitary tumours can be removed using an endoscope (camera) via the nasal passages. If the tumour cannot be removed this way, it is removed via an operation through the skull (Craniotomy). The surgery is performed under general anaesthesia. The surgery itself is performed jointly by an ENT (Ear, Nose and Throat) surgeon and neurosurgeon. The role of the ENT surgeon is to gain access through the nose into pituitary gland. The lining from inside the nose is prepared to cover the defect in bone at the end of operation.
The pituitary tumour is then removed by a Neurosurgeon. The tumours are dissected off of the carotid arteries to the side, and from the nerves to the eyes above. However, in some cases it is not possible to remove all the tumour if it cannot be dissected from the carotid arteries or sensitive tissue around the tumour. In that case, the aim is to remove as much as it is possible safely, whilst trying to preserve function of the gland.The final step is to reconstruct the defect in the skull base. This is done by using a flap of nasal lining to cover the bony defect. If the fluid surrounding the brain (cerebrospinal fluid) leaks out during the operation, the repair is done by using a graft of fat and fibrous tissue (fascia lata) graft from the thigh.
Sometimes it is necessary to repeat the surgery for recurrent tumours or to repair a persistent leak of cerebrospinal fluid. A lumbar drain may be inserted for such a repair.
On the day of surgery
Pituitary – On the day of surgery
You will have received a pre-admission letter that will detail the specific time and location of where you are to attend on the day of surgery.
On the morning of surgery you will be met by our nursing staff who will go through a pre-operative checklist of questions take your baseline observations and prepare you for operation.
You will also meet members of the surgical team who will once again discuss the details of the operation the aims and risks and obtain written consent to proceed furthermore an anaesthetist will also meet you to discuss the general anaesthetic with you.
You may require a brief ct scan on the morning of surgery if not done previously to allow us to use our computer-assisted navigation system during surgery depending on the order of the operation list.
You will then await surgery for either the morning or afternoon you will be taken to the operating theatre anaesthetic room where your surgery is scheduled and will once again meet the anesthetist and other members of staff.
Further checks will be carried out after which you will receive your general anaesthetic if a urinary catheter is required for your surgery this is usually done after administration of your anaesthetic and we would request consent for this prior to receiving your anaesthetic.
After surgery you will go to our theatre recovery area to have a close at one to one-to-one observation.
Prior to being transferred to our award for your post-surgery care this is usually one of our neurosurgery Wards L24 or L25 but maybe in our high dependency unit should we have deemed you to have.
Any risk factors requiring closer observation most patients after pituitary surgery are discharged home the next day unless there is a specific reason to stay longer.
Check list for Next Day Discharge
| Yes | No | |
| Age above 65 | ||
| Coronary stents | ||
| History of being on Antiplatelet, Anticoagulant | ||
| Intradural extension of lesion | ||
| Sleep apnoea | ||
| COPD | ||
| Known diabetes insipidus | ||
| Other significant co-morbidities | ||
| Uncontrolled hypertension | ||
| Renal impairment | ||
| TIA / CVA within last six months | ||
| No accompanying adult carer 48 hours after discharge | ||
| No access to emergency service |
If all of the above is checked, then you are suitable to be discharged home the next day after surgery. Discharge will also be guided by events during the operation.
After your surgery
Pituitary – After surgery
After surgery you may have the feeling of nasal congestion and some discomforts this is to be expected but you will be giving painkillers so this is tolerable on the day.
After surgery you will be met by multiple members of our team you will be seen in the morning junior doctor ward round.
You will also be seen by one of the surgical team involved in your surgery as well as a member of the endocrine team.
After surgery we would expect your vision to be no worse than before surgery and if you feel it is worse or getting worse. Please inform us we are also keen to ensure you have not developed an imbalance of your salt levels after surgery and therefore we need to measure your urine output closely. Please ensure any time you pass urine that the nurses are aware and record the volume.
We will also perform a blood test on the day after surgery to assess your salt levels.
It is expected that you will have some nasal discharge and bleeding after surgery and this will settle over the first few days. If however you are experiencing a leak of clear fluid from your nose or a salty sweet taste in the back of your throat, This may indicate a leak of cerebrospinal fluid csf and you should inform the medical staff.
All being well if there is no concern of a csf leak your vision is stable your salt levels are satisfactory you are mobilizing on the ward.
Uncomfortable we will aim to discharge you home for the next stage of your recovery.
You will usually see myself a mel gerard prior to discharge and we will aim to answer any questions you may have or ask the doctors to address any issues.
After discharge home
Pituitary – After discharge home
Whether you are on steroid replacement therapy called hydrocortisone prior to surgery or not you should continue the prescribed regime.
When you go home and until you are reviewed by the endocrine team the endocrine team will perform blood tests to decide whether the hydrocortisone can then be discontinued or not. It is very important that you do not discontinue your hydrocortisone medication unless specifically told to by your endocrine team and that you arrange a repeat prescription with your GP. In advance of finishing your supply abruptly stopping your hydrocortisone medication could precipitate a medical emergency.
If you are unwell for any reason whilst you are on steroid replacement such as an infection or after an injury it is important to double the dose of hydrocortisone for three days. For further information please refer to the steroid replacement information leaflet you will have been provided.
With to encourage healing within the nose we ask you commence the prescribed nasal irrigation of your nasal passages. From day two after surgery we advise doing this through each nostril twice a day at least until you are reviewed in ent clinic.
At around six weeks after surgery I will usually contact you by telephone in the first two weeks after surgery to see how you are getting on but you will have access to my number found in the information leaflet during this period should you need.
Post Operative Instructions
What to Expect after Surgery:
Headaches & Pain
You will be given a prescription for pain medication. Directions will be on the package. Pain following pituitary surgery is usually readily controlled by medication. Do not be afraid to take a pain pill if you are uncomfortable, especially when going to bed at night or awakening in the morning. Sleeping with your head elevated (on at least two pillows) helps decrease pain and swelling. Do not operate machinery or drive when taking strong pain medication (narcotics).
If your headaches worsen or are unrelieved by pain medication or your neck feels stiff and painful please call the contact numbers given below.
Fatigue
It is normal to feel fatigued after surgery for three to four weeks. Pace yourself. Slowly increase your activity and remember to rest when you are tired.
Sinus Congestion
Don’t be discouraged if you can’t breathe through your nose at first. It typically takes two to three weeks before the inflammation and swelling inside the nose have subsided enough to provide a good nasal airway. If you think you have a sinus infection, please call the contact numbers provided. Initial nasal congestion may cause a temporary loss of taste.
Nasal Drainage
You can expect some bloody mucus drainage from your nose. This drainage will be greatest the first three days after surgery. It is best not to blow your nose immediately after surgery, as this may cause bleeding. After three days, you may blow your nose gently. Clear fluid, like water dripping from a tap, or a lot of bright red blood like a nose bleed is not normal. Please contact us immediately, in that case.
What happens if my nose bleeds?
Spotting of red blood, or bloody mucous, is normal. Brisk bleeding, dripping from the nose that doesn’t stop after a few minutes of sitting up and squeezing your nostrils together is not. This happens rarely, and when it does, it is almost always a small vessel in the nose (not the tumour or brain). Control it with pressure and go to your local A&E. They may have to pack your nose to stop it. Notify us if this occurs.
Cleaning Your Nose
The best way to clear your nose of mucus and dried blood is with Sinurinse irrigation, starting on Day two after surgery. This should be done up to four times every day for up to six weeks. If done correctly, mucus will be flushed out of the front of the nose. Some mucus may even be rinsed to the back of the nose and flow out of the other nostril or the mouth.
Demonstration on using the nasal rinse and DIY recipe
DIY recipe for sinurinse: one pint of cooled down boiled water with one teaspoon of salt and 1/2 teaspoon of bicarbonate of soda.
NeilMed Sinus Rinse
NealMed Sinus Rinse it’s safe simple to use and provides quick relief.
To help you breathe easy before you get started make sure your hands are clean next fill the bottle to the line with lukewarm distilled water or previously boiled water.
Mix in the packet of NealMed Sinus Rinse solution and give the bottle a swirl making sure it’s dissolved standing over the sink then forward and tilt your head slightly down keeping your mouth open and without holding your breath.
Place the cap snugly against your nose squeeze the bottle gently until the solution starts draining from the opposite nasal passage.
Keep squeezing until you used about one half to one quarter of the bottle then blow your nose very gently and repeat on the other side now your sinuses are clear and you can breathe easy.
Sneezing & Coughing
If you need to sneeze or cough during the two weeks after surgery, stay relaxed and let it happen! Don’t hold your breath or pinch your nose!
Avoid things that make you sneeze. Sneezing through an open mouth may be helpful.
Medication and Laboratory Testing
After surgery, you will likely be placed on a low dose of steroid medication (Hydrocortisone). It is important to continue to take this medication daily until you are instructed to stop.
Your endocrinologist will monitor your salt (sodium) and hormone levels in the weeks after surgery. They will instruct you on when and where to obtain the blood tests.
Please refer to Steroid Replacement Therapy Booklet for more information.
Fever
If your fever is higher than 38°C, double your steroid dose until the fever subsides. If during the first two weeks after surgery your fever goes above 38°C, please contact us. Please refer to Steroid Replacement Therapy Booklet for more information.
High Blood Sodium – Hypernatremia
If you begin to pass excessive amounts of urine and become extremely thirsty (awakening multiple times at night, for example), this may be a temporary condition called Diabetes Insipidus.
The pituitary gland may not be releasing enough of the hormone that regulates sodium levels in the blood. Your blood sodium level may be too high – hypernatremia.
You may need regular blood tests after surgery because of this reason. You may need medications until the condition subsides. Please contact the Endocrine nurse specialist to arrange blood tests.
Low Blood Sodium – Hyponatremia
If you are nauseous and have been vomiting, but don’t have a fever, you may have a temporary condition called the Syndrome of Inappropriate Antidiuretic Hormone or SIADH for short. The pituitary gland may be releasing too much of the hormone that regulates sodium levels in the blood. Your blood sodium level may be too low – hyponatremia.
You may need regular blood tests after surgery because of this reason. You may need medications until the condition subsides. Please contact Endocrine nurse specialist to arrange blood tests.
Note that severe hyponatremia is dangerous and can cause seizures. Signs of severe hyponatremia include headaches, dizziness, confusion, lethargy, and an inability to stay awake. Seek immediate medical attention – go to your local emergency department – if this occurs.
Thigh Incision Care
If a graft was used from the thigh, the wound will need the same care as any surgical wound. You may have had some clips on the skin, which would need to be removed in one week’s time at the GP surgery.
If absorbable sutures are used, you will be notified before discharge. If a large swelling or bruise appears on the wound or if you develop a fever and discharge from wound, please contact us.
Showering
You may shower anytime. Cover the thigh incision with plastic when you shower during the first week after surgery. You can get the incision wet after seven days.
Constipation
Pain medication may cause constipation. If you become constipated increase your fiber intake and you may need to take a stool softener or laxative (ducolax, senna, etc).
Bending & Lifting
Heavy lifting, straining, and exercise that might cause bleeding should be avoided during the first two weeks. Don’t be surprised if you tire more easily than usual. Wait for about four weeks before resuming a strenuous exercise program.
Other Activities
- Generally you can return to work in four – six weeks depending on the work you do
- You can jog after two weeks and exercise regularly after four weeks
- You can eat whatever you like and drink to thirst
- You can fly in four – six weeks’ time
- You can drive once recovered from surgery as long as you are not taking narcotic pain medications and depending on your pre-existing visual loss
- You can swim after two weeks and can play golf any time
- There are no restrictions on being sexually intimate with your partner
When to call after surgery
- Fever after the day of surgery higher than 38°C
- Constant clear watery discharge after the first week of surgery – please ring the ward for advice
- Sudden visual changes/loss or eye swelling
- Severe headache or neck stiffness
- Severe diarrhea
- Steady, brisk nose bleeding that doesn’t get better after elevating head / nose pinch
Who to call after surgery
After hours you should call
For endocrine related concerns, please contact your local endocrine nurse specialist. For patients under care of Leeds Endocrinology service
- After two weeks of your surgery, please contact your local GP for advice
- In case of an emergency, please contact your nearest Emergency Department
Follow up (as a guide)
- You will be seen in ENT Clinic in six weeks
- You will be seen in Neurosurgery Clinic in three months
- You will have repeat Goldmann’s Visual Field testing in
- three months
- You will have a repeat MRI scan in six months
- You will undergo endocrine assessment in two – six weeks, with out-patient review shortly thereafter
For further information
Follow up after the surgery
Pituitary – Follow up
The following is what to expect in the weeks and months after surgery the preliminary histology results which is where we look and test the samples from surgery.
Under a microscope will usually be discussed on the next Wednesday multi-disciplinary team meeting.
After your surgery the full results can take up to several weeks you will be followed up by the endocrine team either in Leeds or at your local Hospital.
After a few weeks to assess your hormone function you will be scheduled to be seen in ent clinic around six weeks to assess healing.
In your nose you should receive an appointment to have your visual fields assessed at St James’s Hospital.
In the first couple of months you will be scheduled to be seen by your neurosurgeon in clinic usually in two to three months.
After surgery you should have a post-op mri scan at six months after surgery to assess the removal of the tumor.
The results of this scan will be reviewed in our weekly Wednesday mdt meeting and the decisions regarding ongoing surveillance and follow-up are made there.