What is Long QT syndrome?
Long QT syndrome (LQTS) is a condition of the heart in which the heart takes too long to relax after each heartbeat. It can be inherited as a genetic condition in some people but can also be caused by certain drugs and abnormal salt levels in the body. This page relates to the inherited form of the condition.
Back to topHow common is it?
Long QT syndrome only affects about 1 in 2000 people. It affects men, women, and children. It has been described in families all over the world, but your ethnic background plays a part in how common it is.
Back to topWhat is the “QT” interval?
To understand what causes long QT syndrome you need to know a little bit about how the heart works, how the heart beats and how we measure it on a heart trace – also known as an ECG.
The heart has four chambers – two top chambers called atria, and two bottom chambers called ventricles. Blood is pumped from the atria to the ventricles. The ventricle on the right pumps the blood to the lungs to pick up oxygen and the ventricle on the left pumps the blood all the way around the body.
For the heart to pump blood around the body, an electrical impulse is needed to tell the heart muscle when to contract and relax. This is caused by changes in the levels of salts (ions) either inside or outside of cell walls. It happens automatically and starts in the top right-hand corner of the heart. It spreads over both atria, causing a blip on the ECG called a P wave. The impulse is then channeled through a special signal box in the heart’s centre and down the specialized electrical cells that trigger the ventricles to contract and pump blood.
This causes a sharp spike on the ECG called the QRS complex. The heart then relaxes in preparation for the next heartbeat. This is seen as a broad hump on the ECG called the T wave.
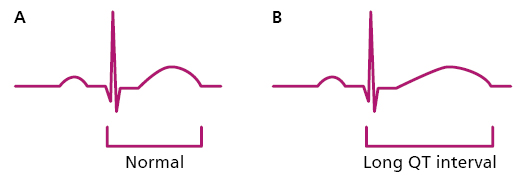
The QT interval simply is a measurement of the time it takes the heart to contract and relax. The electrical impulse is conducted by salts (or ions) that enter and leave the cells of the heart through channels. In people with long QT syndrome, alterations in the genetic code can cause problems in the function of these channels, meaning it takes longer for the heart to relax. We see this on the ECG as a long QT interval.
Figure 1: The heart trace (ECG)
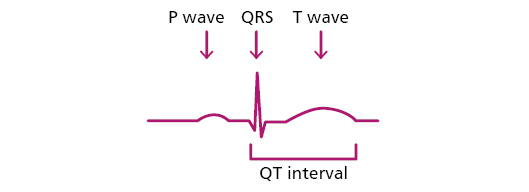
Figure 2: Normal QT interval (A) and Long QT interval (B)
What causes Long QT syndrome?
Long QT syndrome is a genetic condition that can be passed down from one generation to the next. In most individuals (about 60-70%) a genetic alteration (or change in the genetic code) can be detected. Our genetic code (or DNA) is like a list of instructions for how to put our body together. If there is an alteration in the genetic code, this causes a change in how the channel is made and it may not function normally. Several genes/channels are important in long QT syndrome and the three most commonly affected are:
- Potassium gene (KCNQ1) – about 45% of individuals
- Potassium gene (KCNH2) – about 40% of individuals
- Sodium gene (SCN5A) – about 10% of individuals
If the channels are altered, it can affect how the electricity moves through the heart which can prolong the QT interval taking the heart longer to relax. This can lead to abnormal heart rhythms (extra beats, or faster heart rhythms) which can cause symptoms such as palpitations and can sometimes be dangerous.
Back to topInheritance
We inherit our genetic code from a combination of our parents’ genetic codes. One copy of each gene from each parent. An alteration can therefore be handed down from one generation to the next. For most families with Long QT syndrome there is a 50% (one in two) chance that an alteration will be passed on to a child. If you have another child, again there is a 50% (one in two) chance of passing on the alteration. If a person has been diagnosed with Long QT syndrome, in most cases one of the parents will also have the alteration, and there is a 50% (one in two) chance that their brothers or sisters will also have it. It just means that they carry the alteration. Many people with an alteration never have any symptoms and lead perfectly normal lives. If someone has the gene alteration, even though they don’t have any symptoms, they can pass on the alteration to their children.
Back to topWhat symptoms does it cause?
Long QT syndrome does not always cause symptoms. For some, it can cause symptoms such as palpitations or faints.
Palpitations mean different things to different people but in general it is the sensation of a sudden fast heartbeat because of a change in the heart rhythm. Palpitations are common in everyone, not just in Long QT syndrome, so often even if you have this symptom, it will be unrelated to the condition.
The same goes for faints or blackouts. Most people faint at some point in their lives, so fainting is common, but in Long QT syndrome it may be due to a fast and potentially dangerous heartbeat and therefore we take it seriously. It is important that you let us know if you faint.
Back to topHow is Long QT syndrome diagnosed?
Sometimes people are found to have LQTS because of symptoms of faints or palpitations. In other people the diagnosis is made purely by chance – for example if you are having a heart trace (ECG) for another reason a long QT interval may be detected by accident. We sometimes look for LQTS in people who have an affected family member.
Sometimes it is obvious that the QT interval is long, but more often it is a bit more subtle than that. The QT interval varies from day to day depending on several factors including your circulating levels of hormones such as adrenaline.
The QT interval can be difficult to measure on an ECG, and sometimes we need to compare the results over a long time. In a proportion of individuals, the QT interval is within the normal range even though they have long QT syndrome which can make it particularly difficult to diagnose. In this situation we often need to do other tests such as a Holter monitor or an exercise test to unmask the condition (see below).
Back to topWhat tests might I need?
There are several tests we can do in patients with Long QT syndrome.
- ECG: An ECG is a quick test that uses 10 wires or electrodes to record your heart beat for a few seconds. We specifically look to measure the QT interval and the shape of the T wave, which shows how the heart is relaxing.
- ECHO: An Echo (or heart scan) is an ultrasound of the heart and is harmless. We don’t expect to see any abnormalities in Long QT syndrome, but it is a safe way of checking that there are not any other problems with the heart that can mimic Long QT syndrome.
- Holter monitor: A Holter monitor. This is a heart monitor that you take away with you and records your heart rhythm over a period, usually about 24 hours. This is useful if you are having palpitations and to look at how your QT interval varies across the day.
- Exercise test: Sometimes the QT interval is normal on the ECG trace, so we need to do an exercise test to measure the QT interval and see how it changes with exercise. It involves walking and then running on a treadmill with continuous monitoring.
Is there any treatment?
Most patients with Long QT syndrome are unaware of it or have no symptoms. Even if you have no symptoms, it is important to avoid certain medications as these can make Long QT syndrome worse. These include some commonly used drugs like antihistamines for hay fever, certain antibiotics like erythromycin or certain types of heart tablets. A full list will be provided to you but can be found on the website www.crediblemeds.org, and there is a credible meds App which can be downloaded on your smart phone. It is important that you mention this to any doctor prescribing new medication as well as when you buy any medication over the counter.
The main treatment for most people is beta blocker therapy. Some beta blockers are more effective than others in Long QT. The most common are nadolol and propranolol, but others are used. If you need to change beta blockers, you should discuss this with your cardiology team. They are highly effective, and in patients with LQTS give protection against dangerous heart rhythms. They work by preventing your own adrenaline hormones from lengthening the QT interval. beta blockers are common tablets and are very safe. All tablets can have side-effects, but in general, beta blockers are well tolerated in most patients.
If you do have fast heart rhythms or faints, despite beta blockers, then these can sometimes be dangerous. Part of your assessment in the clinic will be to assess your risk of these dangerous heart rhythms, and if we feel you are at risk, we will discuss the option of an implantable cardioverter defibrillator (ICD) with you, or rarely, other procedures that can reduce the risk of you coming to harm.
More information can be found about these devices here:
www.bhf.org.uk/informationsupport/treatments/implantable-cardioverter-defibrillator
Back to topLifestyle advice
It is particularly important to follow certain lifestyle advice to reduce the risk of serious heart rhythm abnormalities.
- Avoid any medicines which can affect the QT interval www.crediblemeds.org
- Avoid excess alcohol.
- In general, you should avoid vigorous and competitive sports. Recommendations for exercise vary depending on how prolonged your QT interval is, which type of LQTS you have, and whether you have symptoms, so please discuss this with your cardiologist.
- If you have LQTS type 1 you should avoid strenuous swimming or diving into cold water.
- If you have LQTS type 2 you should avoid sudden loud noises. Keep mobile phones on a lower volume, and use “crescendo” alarm clocks, which start at a lower volume and gradually increase.
Take action if you experience any of these symptoms:
- If you have diarrhoea and/or sickness, use oral rehydration therapy, such as Dioralyte, which can be bought from a pharmacy or shop, to keep well hydrated.
- If you have prolonged diarrhoea or sickness, go to your nearest urgent care centre for blood tests to check your electrolytes, and an ECG to check your QT interval.
- If you have a blackout you should go to your nearest urgent care centre. Tell them that you have been diagnosed with LQTS.
Can I drive with long QT?
You need to inform the DVLA of your diagnosis, but most people can continue to drive.
You can find the DVLA form at:
www.gov.uk/long-qt-syndrome-driving
If your QT interval is very long (above 500 ms), you must stop driving and inform the DVLA. Once the DVLA has received a report from your cardiologist, you will usually be able to drive again.
If you have a faint, you should stop driving until the cause of the faint has been found and, if necessary, treated.
Back to topPregnancy
Please let your cardiologist know if you are planning pregnancy or become pregnant. Patients with LQTS do not usually have problems during the pregnancy but have an increased risk of heart rhythm problems after the baby is born. You can continue beta blockers during pregnancy but should discuss this with your team.
There may also be reproductive options available if you have a genetic alteration such as testing in a pregnancy or after birth.
Back to topDo my relatives need to be tested?
Long QT syndrome is often an inherited condition and so other family members may also have the condition. We therefore recommend simple tests to check them out so that we can advise them. Each first degree relative (children, siblings, and parents) has a 50% (one in two) chance of carrying the inherited cause, but a lower chance of having the condition itself. It is worth getting tested, but it is an individual choice, and some people prefer not to.
We would see them in the clinic, ask a few standard questions about symptoms and perform an ECG, an exercise test and often a Holter monitor. If these tests are all normal this is reassuring. If the tests showed Long QT syndrome, we would continue to assess them over time in the clinic if necessary and give any specific advice or treatment recommendations.
Back to topGenetic Testing
Genetic testing can be very helpful in some families with Long QT syndrome. It can provide some useful information about which type of Long QT syndrome you may have and if a clear-cut alteration is found, other family members can be tested for the same alteration. This can be helpful in finding those relatives at risk of developing the condition in the future.
Be aware not all families with LQTS have an identified genetic cause so speak with your clinician to find out if genetic testing is a possibility in your family.
Back to topHow can I get further information?
Point of contact for clinical questions
Adults:
Annabel Nixon, Rachel Walker, ICC Nurse Specialists,
Telephone: 07584 184 602
Email: [email protected]
Children
Beth Lunn, Paediatric ICC Nurse Specialist
Telephone: 0113 392 5467
Email: [email protected]
Point of contact for questions about genetics:
Genetic counsellors:
Kath Ashcroft and Kathryn Moore
Telephone: 0113 392 4457 and 07789 003 997
Email: [email protected]
The charities BHF, SADS UK and CRY have information about Long QT syndrome and provide help and support for patients and families.
Their websites are:
- http://sadsuk.org.uk
- www.c-r-y.org.uk/
- www.bhf.org.uk/informationsupport/conditions/long-qt-syndrome