You have been given this leaflet because you have recently been diagnosed with Premature Ovarian Insufficiency (POI).
What is Premature Ovarian Insufficiency (POI)?
A normal menopause is defined as when you experience no menstrual period for 12 months with no other medical explanation. The ovaries stop releasing eggs and the monthly bleed does not occur. There are often other signs such as hot flushes and mood changes as hormone levels change, particularly oestrogen. The average age that the menopause occurs is 51 years.
A menopause occurring under 45 years is considered early and a menopause under 40 is premature. Premature menopause is now more commonly known as Premature Ovarian Insufficiency (POI).
How common is POI?
POI is more common than you may expect, affecting approximately 1 in 10,000 people before the age of 20 years, 1 in 1000 before the age of 30 and 1 in 100 before the age
of 40.
However, recognising POI can be delayed or missed as many people may not present to their doctors or their symptoms are put down to other causes e.g. stress.
What are the symptoms of POI?
The most common symptom experienced is the absence of your monthly menstrual period or having infrequent menstrual periods.
However, you may also experience any of the following symptoms:
Physical
- Hot flushes
- Night sweats
- Heat intolerance
- Palpitations (awareness of heart beat)
- Infertility
- Changes to skin and hair (dryness, thinning)
- Headaches
- Breast tenderness
- Fat redistribution
- Needing to pass urine more often and with more urgency
- Pain passing urine
- Urinary tract infections/cystitis
Psychological
- Mood changes and irritability
- Lethargy
- Difficulty concentrating
- Anxiety/ panic attacks
- Depression
- Sleep disturbance/ insomnia
- Fatigue
- Lowered self-esteem
Sexual
- Reduced sex drive
- Vaginal dryness
- Pain during sexual intercourse (Dyspareunia)
What causes POI?
In most cases of POI, no specific cause is found. This can often be upsetting and frustrating. However, POI can also be due to several medical causes such as:
- Genetic reasons e.g. Turners syndrome.
- Autoimmune conditions (when the body develops an
- intolerance to its own cells such as the ovary).
- Surgical removal of the ovaries.
- Radiotherapy and / or chemotherapy.
Why does POI matter?
What is oestrogen and why is it important?
Oestrogen is the main hormone that is produced by the ovaries, along with progesterone and small amounts of testosterone. Oestrogen is important for fertility and egg production, and with progesterone, it helps to prepare the womb for pregnancy. It also plays an important role in keeping bones strong and the heart and blood vessels healthy.
During the perimenopause (the years before and after the last period) oestrogen levels begin to decline to a much lower level.
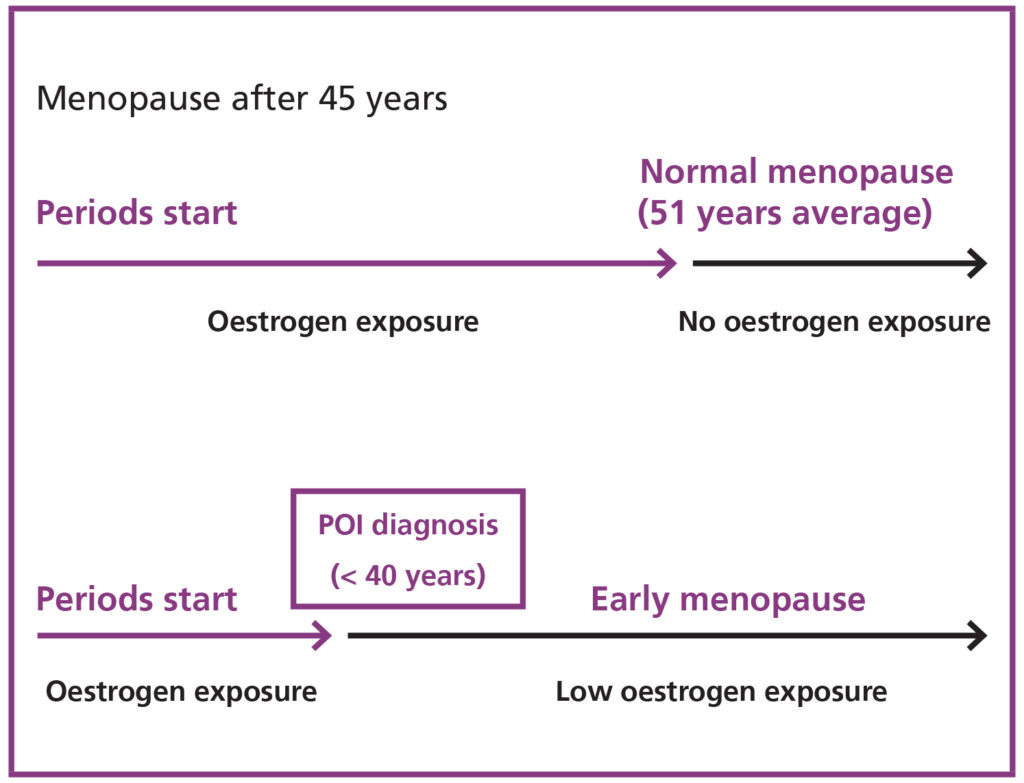
In POI this decline happens earlier and means that individual experiences a longer period of time with oestrogen deficiency. This can lead to the unpleasant symptoms listed above and some long-term health issues outlined below.
Variation of lifetime exposure to oestrogen
If you have early menopause (POI) you spend a longer part of your life with little or no oestrogen.
Are there any long term health complications?
A lack of oestrogen over several years can lead to weakness of the bones called osteoporosis. The bones of the spine can collapse (causing loss of height) and bones in the arms and legs can break more easily because they are brittle. Bone strength (density) can be measured with a special type of scan.
A low level of oestrogen for a long time is linked to heart disease, including heart attacks and strokes. It is thought that dementia may be more common too.
How can I protect myself against these complications?
Replacing the oestrogen is quite easy to do. HRT aims to give you normal levels of oestrogen than your body is unable to produce naturally to prevent or reduce these complications. This not only reduces the risk of long-term complications, but also relieves other menopausal symptoms such as hot flushes.
Hormone Replacement Therapy (HRT)
Hormone replacement therapy (HRT) has been proven to be effective, for reducing symptoms like hot flushes and night sweats experienced in POI. HRT is a treatment that gives back the hormones you are missing. This treatment is recommended until at least the average age of menopause, which is 51 years in the UK.
Oestrogen is given with progestogen (progesterone-like hormone) when your womb is still present. Oestrogen is not given alone because this increases the risk of abnormal changes in the womb lining which can become cancerous. Progestogen effectively protects the womb lining from this side-effect.
Types of HRT available

Womb Present
Pattern of hormones:
Cyclical: Oestrogen alone for 2 weeks followed by oestrogen and progestogen for 10 – 14 days.
Available forms:
Tablets: By mouth daily.
Patches: To stick on the skin (weekly / twice weekly).
Gel: To rub in daily.
Bleeding pattern: Monthly.
Best for:
If you have ambitions to become pregnant one day with a donated egg.
Womb Present
Pattern of hormones:
Continuous: Oestrogen and progestogen.
Available forms:
Tablets: By mouth daily.
Patches: To stick on the skin (weekly / twice weekly).
Gel: To rub in daily.
Bleeding pattern: No bleeding (Occasional spotting).
Best for:
Post-menopause (over 50 years old) no period for more than a year.
Absent (hysterectomy) or progestogen intrauterine system (IUS) in place
Pattern of hormones:
Continuous: Oestrogen only.
Available forms:
Tablets: By mouth daily.
Patches: To stick on the skin (weekly / twice weekly).
Gel: To rub in daily.
Bleeding pattern: No bleeding (Occasional spotting may occur with IUS).
Best for:
After a hysterectomy or if you have an IUS already in who don’t want to take two hormones in other forms.
Is HRT safe for me?
In recent years, there has been alot of publicity about the safety of HRT. This has been exaggerated by bad press of studies claiming to have found a link between HRT and an increased risk of breast cancer and heart disease. This has led to worry about the safety of HRT. However, these studies do not apply if you have POI as they involved a much older age group.
Does HRT increase my chance of getting breast cancer?
No, your risk of breast cancer is no different to a pre-menopausal person of the same age if you take HRT. The risk only increases slightly after the age of normal menopause (51 years old) if you choose to continue taking HRT.
Will I have an increased risk of cardiovascular problems?
The risk of heart disease is NOT increased if you are under 51 years taking HRT. Studies which suggested this were carried out on people over 51 years and some of the original research has now been deemed inaccurate.
Deep Vein Thrombosis (DVT) (blood clot in the leg veins)
There is a slightly increased risk with tablet forms of HRT (as with the contraceptive pill) compared to not taking hormones. The risk of blood clots with patches / gel / spray at a standard dose is not increased compared with people not using them.
Endometrial cancer (cancer of the womb lining)
If you have a womb you should take combined HRT (progestogen and oestrogen) to minimise the risk.
What other treatment options are available?
Other treatments can help to relieve symptoms and improve wellbeing, such as:
- The use of vaginal oestrogen works well for vaginal and bladder symptoms. It is available in creams, tablets and rings.
- Wiping with a cold flannel or having a shower when experiencing hot flushes.
- Various herbal remedies (ALWAYS consult your doctor before commencing these).
- Counselling and support groups.
- Psychosexual advice and support e.g. using lubricating gel / cream.
None of these are substitutes for HRT and they will not protect you against the long term health risks discussed above.
What lifestyle changes should I make?
- Stop smoking – smoking reduces the effectiveness of HRT and is a major risk factor for many health problems including heart disease and high blood pressure, and osteoporosis.
- Decrease alcohol intake – excess alcohol can further reduce bone strength leading to osteoporosis. It also increases your risk of falling which could cause bone fractures. Try to stay under 14 units per week (standard measures of single shot / small glass of wine =1 unit) and fewer most weeks.
- Regular exercise – aerobic exercise helps to reduce cardiovascular risks whilst weight-bearing exercise protects against osteoporosis. Aim for at least 30 minutes on at least 3 days per week.
- Eating a balanced diet – this provides important sources of calcium and other essential vitamins and minerals. Dietary supplements such as calcium and vitamin D may be recommended. Minimise or exclude processed food from your diet (takeaways, ready meals, products with ingredients you don’t recognise on the label, fizzy pop, junk food). Maximise fresh produce and cooking from scratch.
- Sleep – Make a conscious effort to get at least seven hours sleep and build relaxation time into your day.
Can I still have children?
A very distressing consequence of premature ovarian insufficiency is infertility. This does not necessarily mean you will not be able to have children; There is a small chance you may get pregnant naturally after POI has been identified because even a very weak ovary can spark an ovulation at random after some time not working at all. It is rare for this to result in a successful pregnancy, but not impossible.
The majority will, however, be unable to conceive naturally which can lead to feelings of inadequacy or failure. You may be offered, and you can request a referral to see a fertility specialist to talk about your options. Counselling support is available, when you feel you might want to talk about this side of your life.
Despite this there are several options available for you if you cannot conceive naturally.
- In vitro fertilisation (IVF) – as the ovaries have very few or no eggs left it is necessary to use an egg from another person (donor egg) to fertilise with your partner’s sperm, in order for you to carry the pregnancy and birth your baby. This may not suit everyone but it can be very successful (about half who try will have a baby but it may take more than one treatment attempt). There are lots of things to think about with this type of treatment. The fertility clinic will provide lots of help and support.
- Adoption and fostering – this can be a long process but can be extremely rewarding.
- Positively childless – some people choose not to have children. This should be seen as a positive choice (see story below).
Jean’s Story – Jean was diagnosed with POI in her 30’s
“Positively Childless to me means total control of my life. I value freedom and independence and want to accomplish/experience things that would be difficult to do if I were a parent. Not having children is liberating, I am happy and my life is full and exciting.”
Additional resources on these topics can be found below in the ‘useful resources’ section
How do I cope with this diagnosis?
Being diagnosed with POI can be an extremely distressing time. It is normal to feel low and stressed when coming to terms with the diagnosis. It is important to to realise that you are not alone and there are many others going through this. It may be helpful to talk to someone about this or to research the condition further.
Several websites and support groups are available and some are listed at the end of this booklet.
What about contraception?
In POI, sometimes your ovaries go through waves of activity. You can have a few periods and then a gap. This pattern can be repeated. Having a period can be a sign that an ovulation has happened. HRT is not contraceptive so if you want to avoid an unplanned pregnancy you must take precautions. The contraceptive pill can be used as a form of HRT with the same protective benefits of oestrogen, if needed. Other methods of contraception maybe discussed with your GP.
Are there any other hormones that are important in POI?
Testosterone is also produced by the ovaries and levels can fall significantly if both ovaries have been removed. If this occurs, symptoms such as fatigue, low sex drive, low mood and headaches may be experienced. Testosterone replacement can help to relieve these symptoms and can be discussed with your health practitioner.
Informed consent
This leaflet is provided to supplement verbal information that will be given to you by your healthcare provider (Doctor/ Surgeon/ Nurse) as part of the consent process prior to your procedure. Information sharing between you and the clinician is essential to ensure that your decision to consent is fully informed.
Please ask questions if you don’t fully understand or have any concerns about what is proposed. You have a right to be involved in these decisions and should feel supported to do so. Please take the time to consider what is important to you to ensure the information you receive is specific and individualised.
Useful resources
Contact us
If you are concerned about your fertility or wish to discuss starting a family contact the Leeds Centre for Reproductive Medicine.