Transarterial Chemoebolisation is a treatment used for patients who have liver cancer. A shorter name for this treatment is TACE.
On this page
- What is Transarterial Chemoembolisation?
- Who can have Transarterial Chemoembolisation?
- Will I have a general anaesthetic?
- What are the benefits of Transarterial Chemoembolisation?
- Can I be cured?
- What are the risks of Transarterial Chemoembolisation?
- What happens after the procedure?
- How long will I stay in hospital?
- If I agree to this treatment what happens next?
- What happens after I go home?
- Further questions
The commonest cancer treated in this way is Hepatocellular Carcinoma (or HCC). This is a primary liver cancer, meaning it has arisen in the liver, usually because the liver has been damaged over many years and has become scarred (or cirrhotic). Secondary liver cancer means a cancer that has spread from another site. An unusual cancer called a neuroendocrine cancer (NET) that has spread to the liver can be treated with TACE but other secondary cancers cannot be treated in this way. This booklet will focus mainly on patients with HCC, but if TACE has been recommended for NET you may also find it helpful.
What is Transarterial Chemoembolisation?
This is a procedure performed under X-ray guidance which uses a fine, soft, flexible tube to enter blood vessels within your liver so that chemotherapy can be given as close to the cancer as possible. Following that, the blood supply to the cancer is then blocked. The blockage of the blood flow to the cancer is called embolisation.
You will come into hospital for this procedure where you will be admitted by one of the clinical team. Blood tests will be taken to ensure your liver and kidneys are functioning well and to examine your blood clotting ability; if there are abnormalities in your blood clotting or platelet count, you may need a transfusion of blood clotting factors or platelets before the treatment can start.
Normally you will have an intravenous drip to ensure that you are well hydrated before the treatment. The treatment will take place in the X-ray department and is carried out by a team of specialists which includes an interventional radiologist (expert X-ray doctor). The procedure will take approximately one to two hours.
The procedure involves passing a fine tube and wire into an artery (blood vessel) in your groin under X-ray guidance, through a very small hole that is made after the area has been numbed; this is called a ‘transarterial’ method. From here tubes and wires are passed into the arteries going into your liver, but you should not feel these inside you. X-rays are taken to identify the blood vessels supplying the tumour by injecting X-ray dye (contrast) into the tube.
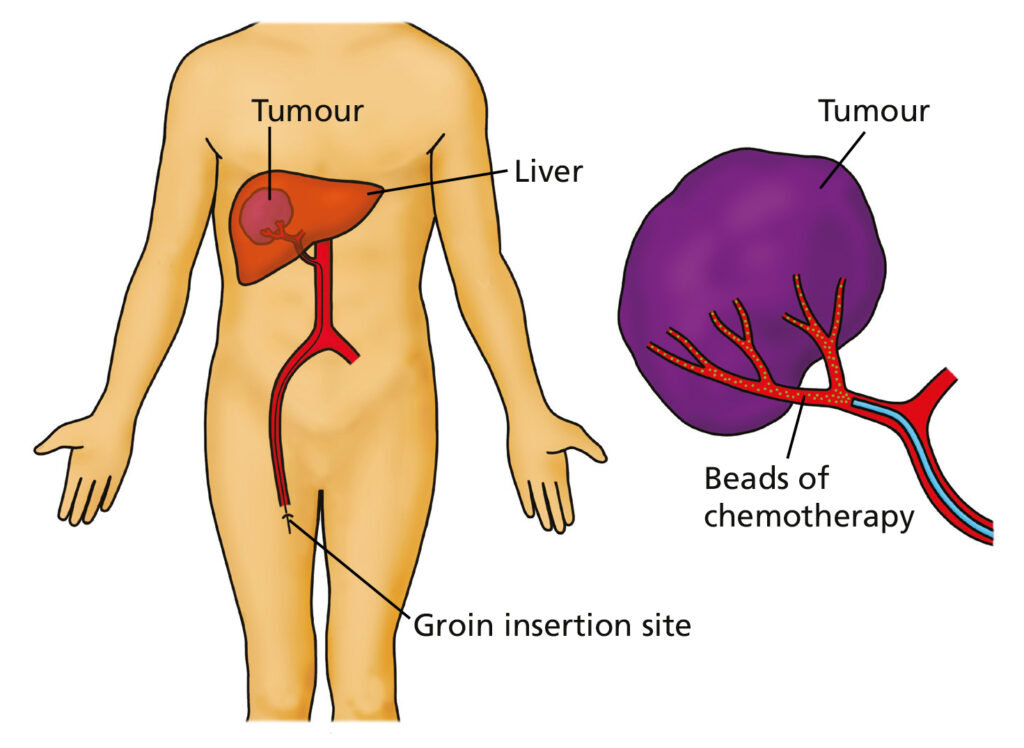
The X-rays allow us to see where in the liver the cancer is and identify which arteries are supplying the cancer. If it is safe and possible to do so, the doctor will then inject cancer killing chemotherapy drugs directly into the cancer and stop the blood supply to the cancer by injecting small beads into the arteries (embolisation). It may take two or more separate courses of treatment to treat the tumour.
Who can have Transarterial Chemoembolisation?
Unfortunately not everyone with a liver cancer can have this procedure. Your cancer has to have started in the liver and your liver must be working well in order to withstand both the chemotherapy and the ‘blocking-off’ of the blood supply to the cancer within the liver.
We know from studying patients around the world that this procedure is only successful in patients whose cancer is of a certain size or stage and has not spread to sites outside the liver.
Will I have a general anaesthetic?
No, this is unnecessary. You will have a local anaesthetic injection around the site of the blood vessel, before the tube is inserted. Usually this is an artery in the groin area, but occasionally an arm artery may be used.
You will also receive strong pain killers which may make you feel sleepy. These can sometimes make you feel nauseated but this can be treated with anti-sickness medication.
What are the benefits of Transarterial Chemoembolisation?
The purpose of TACE is to reduce the size or rate of growth of the cancer and to improve your life expectancy. Studies from around the world have shown that transarterial chemoembolisation can be successful in controlling the cancer that is in your liver and delays the cancer progressing. In achieving this patients with primary liver cancer who under go the procedure live longer.
Can I be cured?
Unfortunately we do not believe that we can cure your cancer with TACE although we are aiming to control your cancer so that you will live longer.
What are the risks of Transarterial Chemoembolisation?
The risks and side-effects of this treatment are due to the two parts of the procedure. Fatigue is a very common symptom after this procedure. Almost all people having this procedure experience a feeling of general tiredness lasting for around two weeks. This is normal.
1. Chemotherapy
There is a risk that the chemotherapy does not just stay in your liver but moves into your blood stream, very rarely causing hair loss and a sore mouth. It may also suppress
your bone marrow which could make you more vulnerable to infection (usually from bacteria inside your body and not from outside sources). These side effects are temporary and are rare.
2. Embolisation
Common risks:
The most common side-effects from this treatment are a cluster of symptoms called post-embolisation syndrome. About half our patients experience this to some extent. The symptoms are similar to having flu, such as shivers, shakes and a mild fever. Other symptoms include pain or discomfort in the upper abdomen, being more tired than usual and going off your food. This is because your body is coping with the dying tumour cells. These symptoms are often helped by taking rest, eating smaller meals more often and taking painkillers.
A lot of pain is uncommon after the first day or so. Overall these symptoms may last up to two weeks and can be associated with a slight temperature.
You will be given strong pain killers for a few days after your treatment to help with this. Regular doses of paracetamol will help, however, if you are worried about your symptoms, please do not hesitate to get in touch with your HPB nurse specialist on:
Or contact your GP or NHS 111.
Uncommon/Rare:
There is a small risk of bleeding from the needle site in your groin. This is generally controlled by pressing on the spot for a few minutes.
A bruise in your leg is not uncommon for a week or two after treatment. It will be necessary for you to stay in bed for around 4 – 6 hours after the procedure to help the needle site in the groin to heal. Rarely, the bleeding is more serious and other treatment is required.
There is small risk of damage to other arteries in your body or leg by the movement of the tube (catheter) inside them. Sometimes this can prevent the chemo-embolisation treatment from being finished.
The embolisation part of the treatment can occasionally cause damage to your gall bladder. This can be painful. Damage to the bile ducts (these are the pipes which drain the bile around and from your liver) is uncommon. This damage may require a further procedure to insert tubes into your bile ducts.
There is a risk that an abscess may form in your liver after the treatment which would require you to be treated with antibiotics and possibly a tube placed into your liver to drain the abscess.
There is a small risk that your liver will not cope with the treatment and then it will fail to work. Liver failure can vary from mild to very serious and can be something from which you may not recover.
Impairment of kidney function can occur following the treatment. This can be due to the contrast, the anticancer drug or dehydration. You will normally have a drip placed before the procedure. This is to ensure you have sufficient fluids to reduce the risk of problems with your kidney function. Overall, serious complications are rare.
What happens after the procedure?
At the end of the procedure the tube is removed from the groin and pressure applied to the puncture site for about 10 minutes to prevent bleeding. A nurse will then escort you back to the ward. You will need to lie flat in bed for 4 – 6 hours. The ward staff will check you at regular intervals during this time.
How long will I stay in hospital?
You will need to have this treatment at St James’s Hospital in Leeds. You will often be admitted the day before the procedure. The average length of stay is 2-3 days.
If I agree to this treatment what happens next?
You will be given a date (usually around 4 – 6 weeks’ time) to come into hospital.
We will discuss the procedure with you and if you haven’t already done so, we will ask you to sign a consent form.
There will be further safety checks that need to be done and we may need to assess you right up to the day of your planned procedure before we can decide whether it is safe. We may not be able to perform chemoembolisation because it would be too dangerous for you.
What happens after I go home?
You may feel tired and quite weak when you go home. If you still have some discomfort from your treatment, continue to take painkillers. A scan of your liver will be performed usually about 4 – 6 weeks after the final course to assess the response to treatment and assess the need for any further treatment.
If you haven’t received an appointment for your follow up scan after four weeks please contact the HPB nurse specialists on 0113 206 8601.
A clinic appointment will be sent to you, if your appointment is scheduled before your scan please can you inform the HPB nurses (on the number above) so your clinic appointment can be rescheduled.
Further questions
We have tried to answer the most frequently asked questions. However, everyone is different. If there is anything you would like to know please do not hesitate to ask. You can contact the HPB nurses: