You have been referred to our service to explore Uterine Artery Embolisation (UAE) as a possible treatment option for your fibroids.
This leaflet outlines the procedure, its benefits, risks, and alternative treatments. Details on recovery from the procedure are also included
What is uterine artery embolisation?
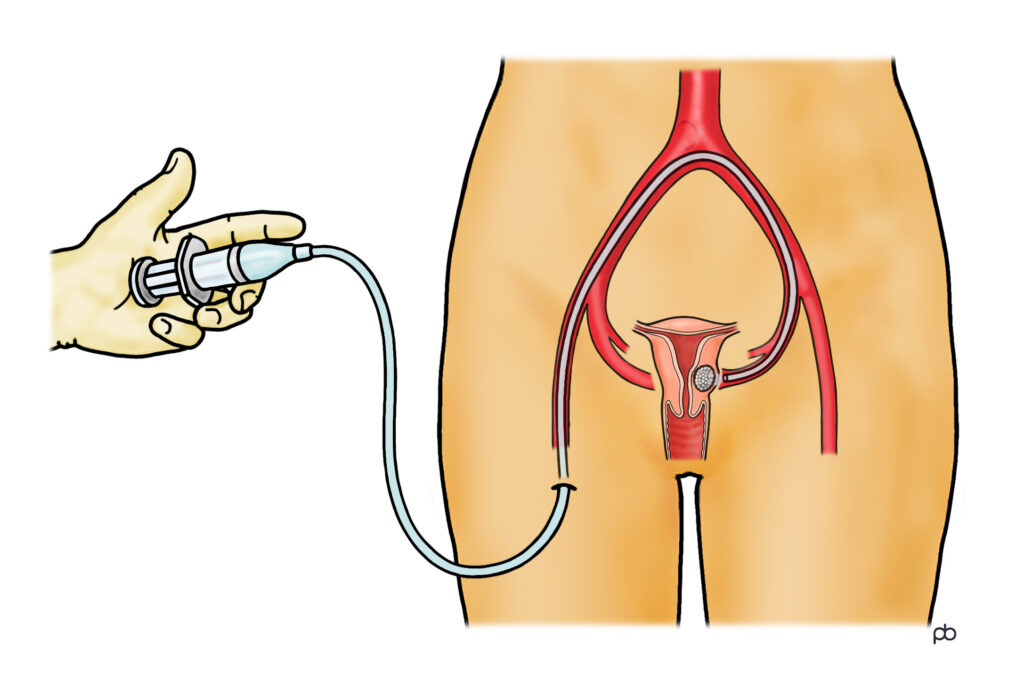
Uterine artery embolisation is a minimally-invasive operation used to treat fibroids by blocking their blood supply so that they shrink over time. It is an alternative to surgery and is performed by an interventional radiologist.
How is uterine artery embolisation performed?
Anaesthetic
The procedure is performed under local anaesthesia.
Operation
A small tube (catheter) is inserted into an artery in the wrist or the groin and guided to the arteries supplying the uterus.
Tiny particles are injected to block the blood supply; this is called embolisation.
The operation usually takes 60-90 minutes.
Pain immediately after the procedure could be significant, often requiring strong painkillers. Patients are kept in hospital overnight for pain relief and observations.
Consent
You will meet the interventional radiologist in clinic (either virtual or face-to-face) to counsel you about UAE. On the day of your operation, you will meet the operating radiologist, who will provide explanation in detail, along with the risks and intended benefits before you provide your permission to proceed via a signed consent form.
What are the risks?
Common/expected effects
- Lower abdominal pain, fatigue and flu-like symptoms for up to two weeks
- Vaginal discharge for up to two weeks, and may last longer in some cases
- UAE uses X-rays (a form of radiation) to visualise the blood vessels to the uterus. We are all exposed to low levels of natural radiation as part of our everyday lives and medical x-rays give an extra dose of radiation. This may increase your chances of developing cancer many years or decades after the exposure. The chances of this happening as a result of this procedure are considered to be very low. It is important to remember that your doctor thinks that the benefits of this procedure outweigh any risks from the radiation. We will make sure that the amount of radiation used in your procedure is as low as possible.
Specific risks
- Risk of hysterectomy (i.e., surgical removal of the womb, which is rarely an emergency) about 0.1% within 30 days
- Approximately 1% risk of non target embolisation to the ovaries, which may cause biochemical menopause. This refers to significant hormonal shifts that happen as ovarian function ceases and characterized by the end of menstruations and various physical and mental symptoms
- Other non target embolisation (e.g., to the bladder) is very rare
- Rare risk of vessel damage requiring emergency surgery
- If the procedure is done from the wrist, there is a very small risk of causing a stroke
Are there alternative investigations / treatments?
A hysterectomy is a major surgery to remove the uterus (womb), often with the cervix, and sometimes the ovaries and fallopian tubes, performed to treat conditions like fibroids.
A myomectomy is a surgical procedure to remove uterine fibroids (non-cancerous growths in or on the uterus) while leaving the uterus intact. Methods vary from open surgery (abdominal) to minimally invasive (laparoscopic/keyhole or hysteroscopic via the cervix).
Hormonal treatments (e.g., GnRH analogues) work by manipulating hormone levels (estrogen and progesterone) to control symptoms like heavy bleeding and to shrink fibroids.
Conservative management refers to monitoring symptoms without intervention if they are mild. Fibroids typically regress (shrink) after menopause when hormone production stops.
What to expect from this operation?
Admission
You will be seen in clinic by an interventional radiologist. If you and the doctor decide that UAE is the right treatment for you, we will schedule the procedure and guide you through the necessary pre-operative steps. You will be contacted by our booking team to offer you an appointment for your UAE. You will then be sent an appointment letter from us detailing your admission. You may be admitted the day before or on the morning of your operation (usually via ward J23).
On the day of your operation, the radiology team may consist of:
- Consultant Interventional Radiologist
- Resident Interventional Radiologist
- Radiology Nurses and Support Workers
- Interventional Radiographer
- Clinical Nurse Specialist
Pre-operative preparation
Any required investigations, including blood tests, will be arranged either by the interventional radiology team or through the pre-assessment clinic.
If you take blood-thinning medications (such as apixaban or warfarin), these will usually need to be stopped before the procedure. If you are receiving injections or other hormone treatments to manage heavy bleeding (such as Zoladex), these may also need to be paused in advance. You will be given individualised instructions about which medications to stop, when to stop them, and when to restart them. If you have not received clear instructions, please contact us well in advance of your appointment to avoid cancellation.
If you have an intrauterine contraceptive device (IUCD/IUD, including Mirena), this should ideally be removed by your GP before the procedure. You may need to use an alternative form of contraception in the meantime.
You will be screened for MRSA and given a five-day course of antimicrobial body and hair wash and nasal ointment immediately before the procedure. Instructions will be provided by the interventional radiology or pre-assessment team.
You may need to fast for six hours before the procedure. This includes avoiding solid food, milk, fizzy drinks, tea or coffee, chewing gum, and similar items. You may continue to drink clear, unflavoured fluids up to two hours beforehand.
On arrival in theatre, you will receive pre-operative medications, which typically include a patient-controlled analgesia (PCA) pump for pain relief, intravenous antibiotics, additional analgesia, and anti-sickness medication. You will be shown how to use the PCA pump before the procedure begins.
Recovery
After the procedure is completed, you will be transferred to the recovery area for monitoring. Moderate to severe cramping pain is common for several hours after the procedure. You will be encouraged to use the PCA pump to control your discomfort, and additional pain relief or anti-sickness medication can be given if needed. Most patients find that the pain improves significantly by the following day.
Aftercare
Back on the ward, the nursing staff will continue regular monitoring. You will be encouraged to eat and drink as tolerated to support your recovery. A radiology or gynaecology doctor will review you and plan your discharge. Most patients go home the day after their UAE.
Care at Home
We recommend that someone is at home with you on your first night after discharge. The following advice will support your recovery:
- Medications: You will be advised when to restart your regular medication. Please take pain relief as advised; if your pain is not controlled, contact us or your GP. Constipation is common with painkillers. Use the prescribed laxatives if needed.
- Nutrition and hydration: Maintain a balanced diet and drink 2-3 litres of water daily.
- Exercise: Start with gentle activity. Avoid strenuous exercise or heavy lifting for 2-3 weeks.
- Work: Most patients return to work after 10–14 days, although some may need longer.
- Driving and travel: Avoid driving for three days after UAE and only resume driving when you feel well enough to perform an emergency stop safely.
- Follow-up: You will receive telephone follow-up at two and eight weeks, and a clinic appointment at six months.
Results
For heavy menstrual bleeding, around 95% of women are satisfied with the improvement in their symptoms after UAE. About 75% of women experience relief from bulk-related symptoms, although this may take up to six months to develop. Symptoms recur in approximately 25% of women within seven years, particularly if menopause has not occurred during that time.
Contact information
We hope some of your questions have been answered by this leaflet. If there are any questions you would like to ask before you come for your operation, please get in touch.
Or contact your GP / telephone 111.
Or attend your nearest A&E department / telephone 999.
How to get to our department
Interventional Radiology is located in the Lincoln Wing of St. James’s University Hospital, Ground Floor.
For directions, please follow this link