Hypoglycaemia (low blood sugar) and Ketotic Hypoglycaemia
Hypoglycaemia is having a blood glucose (also known as blood sugar) level that is too low to provide energy for the body’s cells.
Back to topWhat is glucose?
Glucose is a sugar that is made from the breakdown of carbohydrates found in foods. It is the main source of fuel for the body. It may be stored in the liver and muscles for later use, but spare glucose is converted to fat.
Back to topWhat is a healthy range of blood glucose?
The normal range of blood glucose is around 3.5 – 6 mmols/litre. However, children with a diagnosis of ketotic hypoglycaemia will aim to keep blood glucose above 4mmol. Your child’s doctor will talk with you about what should be a normal range for him or her.
Back to topWhy is hypoglycaemia a concern?
The brain depends on glucose, and too little can affect its ability to function. Severe or prolonged hypoglycaemia could result in fits or serious brain injury.
Causes of hypoglycaemia in young children
Single episodes:
- Sickness and diarrhoea, or another illness that may cause them to not eat enough
- Fasting for a prolonged period of time
- Prolonged exercise with lack of food
What is Ketotic Hypoglycaemia?
Ketotic hypoglycaemia is a common reason for low blood glucose in young children, generally following a long period of time without food. It usually first appears when a child is between 18 months and five years old.
Children with a diagnosis of ketotic hypoglycaemia are more likely than others to have hypoglycaemia during illness, after having fasted (overnight, for example) and after strenuous exercise. Children generally have less muscle mass compared to adults.
This illness causes hypoglycaemia and a build-up of ketones in the body’s tissues and fluids (ketosis). Ketones are chemicals made when supplies of sugar to the body are low and the body must break down fat for energy. Ketones collect in the urine and the doctor can test for them. Other tests are usually done during the first or second episode to make sure your child does not have another reason for low blood glucose.
Back to topTreatment
- Avoid prolonged periods of fasting. It is extremely difficult to determine the exact timescale as this varies with age and severity of Ketotic Hypoglycaemia. We should suggest that if there is a change in standard meal pattern or a skipped meal, then this should be considered as significant.
- Give them frequent small meals and snacks, especially before bedtime
- Bedtime snacks that are rich in starchy carbohydrates e.g. milk, toast, cereal or banana, should be given
- If your child is underweight, nutritional supplements may also be given
Hypoglycaemia is more of a problem during acute illness when your child may not eat well and the body is under stress. You will have been given an emergency regime to give your child when they are unwell to prevent their blood glucose falling.
Back to topSymptoms of low blood sugar
While each child may experience symptoms of hypoglycaemia differently, the most common include:
- Shaking and dizziness
- Sweating
- Hunger
- Headache
- Irritability
- Pale skin colour
- Sudden moodiness or behavioural changes, such as crying for no apparent reason
- Clumsy or jerky movements
- Difficulty paying attention, or confusion
- Tingling sensations around the mouth
Management Plan
What to do if your child is showing signs of low glucose and you do not have access to a blood glucose meter?
If you notice the above symptoms you should give your child foods high in carbohydrate or a drink rich in sugar e.g. Lucozade energy or glucose tablets
If you have access to an emergency regime then this should be started when they first show signs of being unwell. Your child should start to feel better within 10 – 15 minutes of eating or drinking something.
If your child does not respond to having something to eat/drink, or their emergency regime because they are too drowsy, refusing to eat/drink or vomiting, they should be offered a glucose gel (Dextrogel or Glucogel) and taken immediately to hospital.
The amount of gel to be given is detailed below:
Child up to five years
5 grams (1/2 tube of 40% oral gel) and repeated after 15 minutes if necessary.
Child 5 – 11 years
10 grams (1 tube of 40% oral gel) and repeated after 15 minutes if necessary
Child 12 – 17 years
15 grams (1.5 tube of 40% oral gel) and repeated after 15 minutes if necessary
If you have open access to the CAT Unit please contact the nurse coordinator on 0113 392 0921.
If they are unconscious, call 999 for an ambulance.
Back to topOngoing management
If your child has recurrent episodes of hypoglycaemia, then please bring it to the attention of your paediatrician. There are food supplements and medications that can be started. This is usually with guidance from the local Paediatric Dietetic team and the Paediatric Metabolic and Endocrinology team from Royal Manchester Children’s Hospital.
The problem usually disappears on its own by the time your child is 5 – 7 years old and until then the hospital will regularly review your child and advise what to do and who to contact if your child is unwell.
Back to topTreating symptoms of hypoglycaemia
The amount of carbohydrate (CHO) required will depend on the size of the child. If you do not check your child’s blood glucose levels and they are showing symptoms of hypoglycaemia you can use the following to raise the blood glucose levels.
One
Child is unconscious Call 999
Two
Follow treatment plan
Three
Child not showing any symptoms – no action needed
As a guide approximately:
- 5g of glucose is needed for a 10kg child
- 10g of glucose is needed for a 30kg child
- 15g of glucose is needed for a 50kg child
- (Approximately 0.3g/kg)
The amount of carbohydrate (CHO) required will depend on the size of the child. If you do not check your child’s blood glucose levels and they are showing symptoms of hypoglycaemia you can use the following to raise the blood glucose levels.
The following items are good examples:
| Food | 5g CHO | 10g CHO | 15g CHO |
| Lucozade Energy Original | 60ml | 120ml | 170ml |
| Full sugar cola | 50ml | 100ml | 150ml |
| Lift Glucose tablets (round) | 1 tablet | 2 tablets | 4 tablets |
| Glucose tablets (square) | 1 ½ tablets | 3 tablets | 4 ½ tablets |
| Jelly babies | 1 | 2 | 3 |
| Fruit pastilles | 2 | 3 | 5 |
| Honey | 1 level teaspoon | 1 ½ level teaspoons | 2 level teaspoons |
| Jam | 1 level teaspoon | 2 level teaspoons | 3 level teaspoons |
1 x 25g tube of Glucogel = 10g carbohydrate
Chocolate is not recommended as an effective treatment for hypos as the body takes longer to break down the lactose found in milk than it does glucose. The presence of fat further slows the rate of absorption.
Back to topDaily management of ketotic hypoglycaemia
What is a starchy carbohydrate and why is it important?
Starchy carbohydrates are foods such as potatoes, bread, rice, grains, pasta, cereal products, wraps, pitta bread, chapatti, naan bread or crackers. You should try to choose foods that are high fibre and wholegrain varieties where possible. Choose wholewheat pasta, brown rice or leave skins on potatoes. These foods should make up just over 1/3 of the food we eat.
Starchy carbohydrates release energy into the blood more slowly and help keep blood glucose levels stable. It is especially important that children with Ketotic Hypoglycaemia have a supper snack rich in starchy carbohydrate as this will help them maintain their blood glucose during their overnight fast.
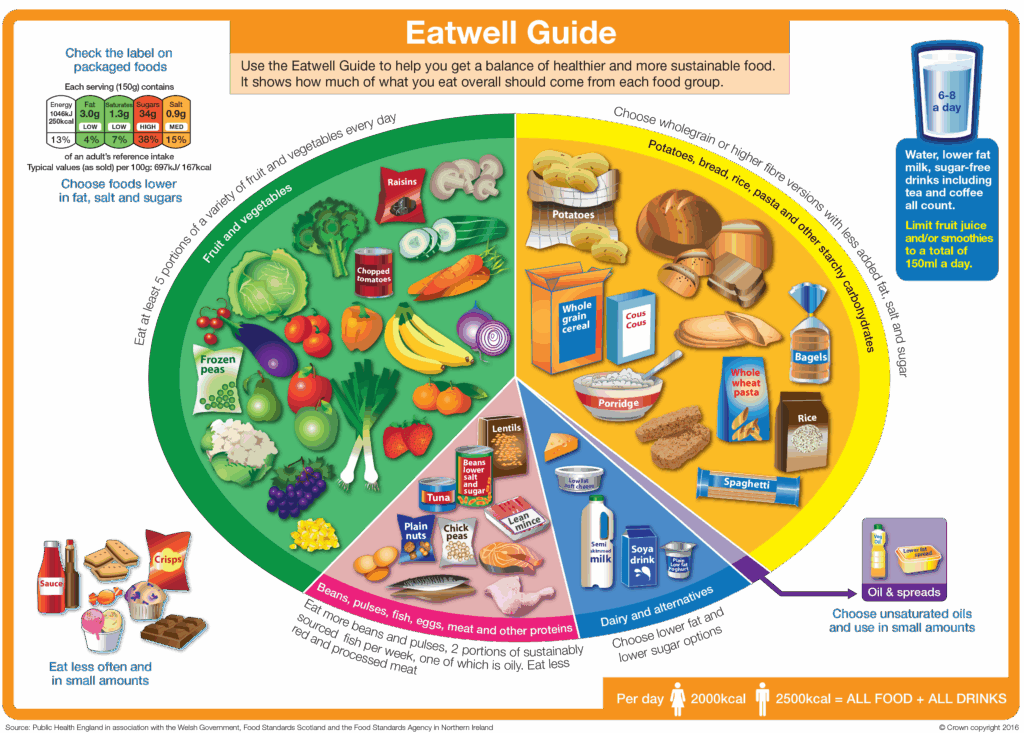
The Eatwell Guide shows the proportions of the main food groups that form a healthy, balanced diet. Here are the main points from the Eatwell Guide:
- Eat at least five portions of a variety of fruit and vegetables every day
- Base meals on starchy carbohydrates such as potatoes, bread, rice, pasta, choosing wholegrain varieties where possible
- Have some dairy or dairy alternatives (such as soya, oat, nut versions); choosing lower fat and lower sugar options
- Eat some beans, pulses, fish, eggs, meat and other proteins (including two portions of fish every week, one of which should be oily)
- Choose unsaturated oils and spreads and eat in small amount
- Drink 6-8 cups/glasses of fluid a day
Children with Ketotic Hypoglycaemia usually only have problems with their blood glucose when they become unwell.
It is important that their diets are well balanced and they have regular meals and snacks. Each meal and snack should contain some starchy carbohydrate foods.
Back to topMeal Ideas
Breakfast
- Shreddies with raisins and milk
- Weetabix with chopped banana and milk
- Cereal bar and banana
- Wholemeal toast with margarine and marmalade
- Porridge/Ready Brek made with milk and dried fruit, e.g. raisins/sultanas
Main meal
- Wholemeal roll/bread or pitta with ham and tomato/tuna and sweetcorn/egg and salad
- Baked beans on wholemeal toast
- Vegetable pizza and salad
- Lentil soup with wholemeal bread/roll
- Fish fingers, mashed potatoes and peas
- Jacket potato and beans/tuna/cheese
- Sandwich, wrap or pitta bread with protein filling
- Chilli con carne with brown rice
- Spaghetti bolognese with wholemeal pasta
- Stir fry chicken and vegetables with brown rice/noodles
- Meat casserole with vegetables and jacket potato
- Fish, chips and beans/peas
- Chicken goujons, potato wedges and beans
Desserts and snacks
- Malt loaf
- Cereal bar
- Fruit cake
- Wholemeal scone
- Flapjack
- Crackers and soft cheese
- Hummus and breadsticks
Nursery/school management
As your child has Ketotic hypoglycaemia, if they fast for a long period of time they can drop their blood glucose levels. If this happens in Nursery, we recommend that your child is offered some foods high in carbohydrate or the emergency regime.
Your child does not need to have their blood glucose checked in nursery/school. If your child has symptoms they will need to treat as per the table above.
If your child does not respond to this treatment or is unable to eat or drink because they are too drowsy, refusing to eat or vomiting they should be offered a glucose gel (Dextrogel or Glucogel) and taken immediately to hospital.
If they are unconscious, call 999 for an ambulance.
Back to topContact us
If you need further advice, please contact:
CAT Unit: 0113 392 7409 / 8929
Paediatric Dietitians (Mon – Fri. 8am – 4pm): 0113 392 0623