The three-dimensional models created by a biomedical engineer at Leeds Teaching Hospitals NHS Trust (LTHT) are helping improve outcomes for patients with congenital heart defects.
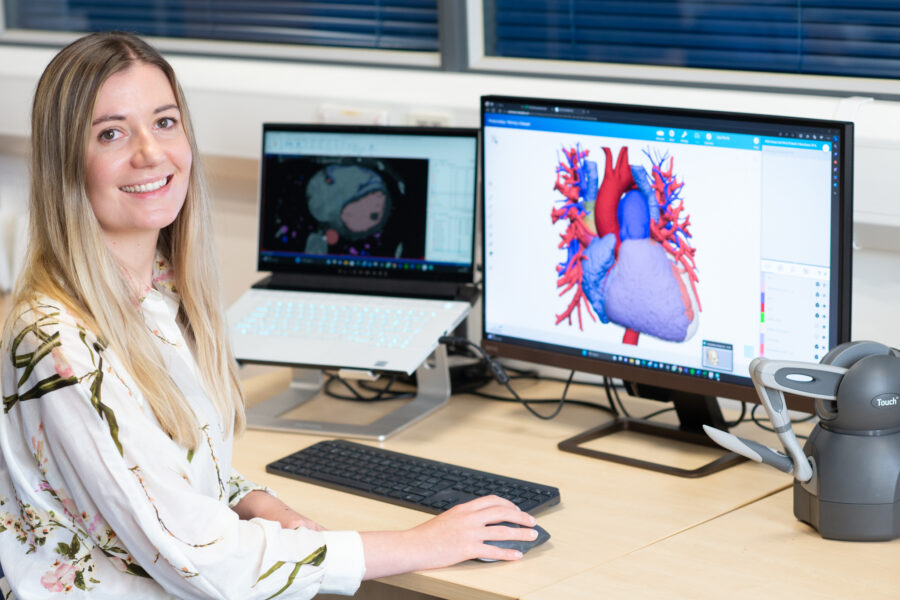
Using computer-aided design, the engineer uses scans of a patient’s heart and turns them into a 3D replica that can be explored and studied on a computer screen.
Clinicians can view the computer-generated model in augmented 3D using a Virtual Reality headset or even request a 3D-printed model. It means clinicians can get hands-on with a reliable replica of the patient’s anatomy to visualise and test surgical approaches before committing to an intervention.
For some conditions, this can make all the difference between someone having to undergo open heart surgery or having a far less invasive stent – procedures which have vastly different levels of risk, and days spent in hospital, and recovery times.
Lisa Ferrie, Biomedical Engineer and 3D Planning Service Lead at LTHT, is the only employee at the Trust to have this unique role, which she started in October last year. She said: “3D modelling provides a detailed level of visualisation that a CT or MRI scan simply can’t provide alone, and leads to safer procedures more suitable to the patient’s individual needs.
This innovative approach means that surgeons are able to make more informed decisions on the best surgical procedure for a patient, with the potential to lead to faster recovery times and less chance of the patient needing further surgery.
Lisa is involved from the start of a patient’s case, working alongside the congenital cardiac team to provide a detailed model replica of patient’s heart. Her model offers a deeper understanding of the patient’s personal anatomy, which widens the treatment options available to patients, including the potential for less invasive approaches.
“It’s a relatively new field,” Lisa explained, “but the potential of this work to improve patient outcomes is huge. More and more you are seeing biomedical engineers or other technical specialists brought in-house to start similar services elsewhere in the NHS.”
Clinicians may also request a model that features a simulated intervention, such as a stent or a synthetic conduit which is used to redirect blood flow.
The models can be viewed digitally, or they can be 3D-printed using a Polyjet printer to provide fully three-dimensional physical models where this is an advantage to the surgical team.
For some conditions, and if appropriate for the patient’s anatomy, a stent procedure can be carried out instead of an open heart intervention. This has significant outcomes for the patient, including fewer days spent in hospital, significantly quicker recovery times, and reduced risks compared to open heart procedures.
Dr Vitor Ramos, Consultant in Adult Congenital Heart Disease and Cardiac MR at LTHT, said: “The 3D designs have a tremendous effect on the way we treat our patients as it provides us with a far better understanding of their anatomies, allowing us to shorten procedures and reduce complications, where appropriate. It also gives us the means us to perform ‘virtual’ surgery beforehand and predict the results of several interventions without putting patients at risk.”
The 3D model becomes an integral part of the information used by the patient’s surgical team to determine what is the most appropriate treatment for each patient. This balances the risk and benefit of each possible intervention and ensures the patient receives the intervention that will provide the best possible outcome.
Ms Carin van Doorn, Consultant Congenital Cardiac Surgeon at LTHT, said: “The 3D modelling service allows us to create individualised heart models for our patients and we use these to plan, and sometimes also practice, the surgical procedure. This advanced preparation is particularly helpful for cardiac surgery as at the time of the operation the heart can be stopped for only a limited amount of time and also the views of the inside of the heart may be restricted. The 3D models are also very useful for our trainees to help understand the many different congenital heart abnormalities.”
Dr Jamie Bentham, Consultant Interventional Paediatric and Adult Congenital Cardiologist at LTHT, said: “The 3D planning service is an invaluable part of the intervention service and allows us to make in-depth assessment and treatment plan prior to a case. It has become a critical part of increasingly complex procedures. The 3D models have become essential for patient safety, equipment choice, procedural suitability and planning procedural steps. We can minimise the risks, reduce radiation dose, and improve the likelihood of success.”