This booklet explains ovulation induction (OI) and intra-uterine insemination (IUI) treatments.
What is ovulation?
Ovulation is the release of an egg in the middle of your menstrual cycle. An egg contains half of the genes needed to make a baby. The sperm provides the other half. You are born with many more eggs than you can ever ‘use’ or ovulate.
You are born with about one million eggs yet the maximum number that could ever be ovulated is about 450, if you never get pregnant and never take contraceptives to stop ovulation. Every day, about 30-40 eggs leave the dormant store in the ovary and begin the journey towards ovulation. Most fall by the wayside and never mature fully. Only one egg reaches maturity each month for ovulation. Usually the rest disappear.
The ovaries contain eggs but they also produce hormones from puberty onwards. Hormone production changes during the menstrual cycle with the development of the ovulating egg. Other cells in the ovary produce hormones that affect the development of healthy eggs (e.g. oestrogen & testosterone).
The ovary itself is controlled and influenced by other hormones. The pituitary gland (master gland) in the brain is crucial to the cyclical pattern of periods. It releases Follicle Stimulating Hormone (FSH) to kick start the development of the monthly egg-containing follicle and Luteinizing Hormone (LH) to trigger the release of the mature egg (ovulation).
FSH and LH hormones released from the brain into the blood stream to stimulate egg development and ovulation.
Oestrogen and progesterone released from the ovary into the blood stream to stimulate the womb lining.
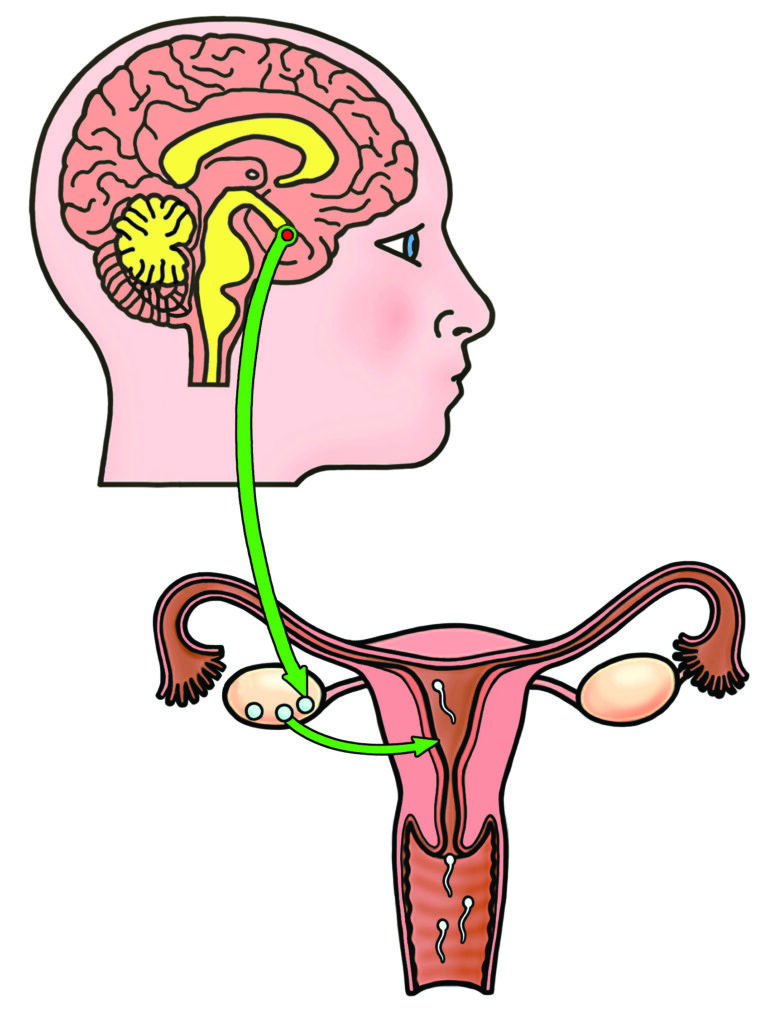
Sperm meet the egg in the Fallopian tube where fertilisation happens.
The embryo travels into the womb to implant 5-7 days later.
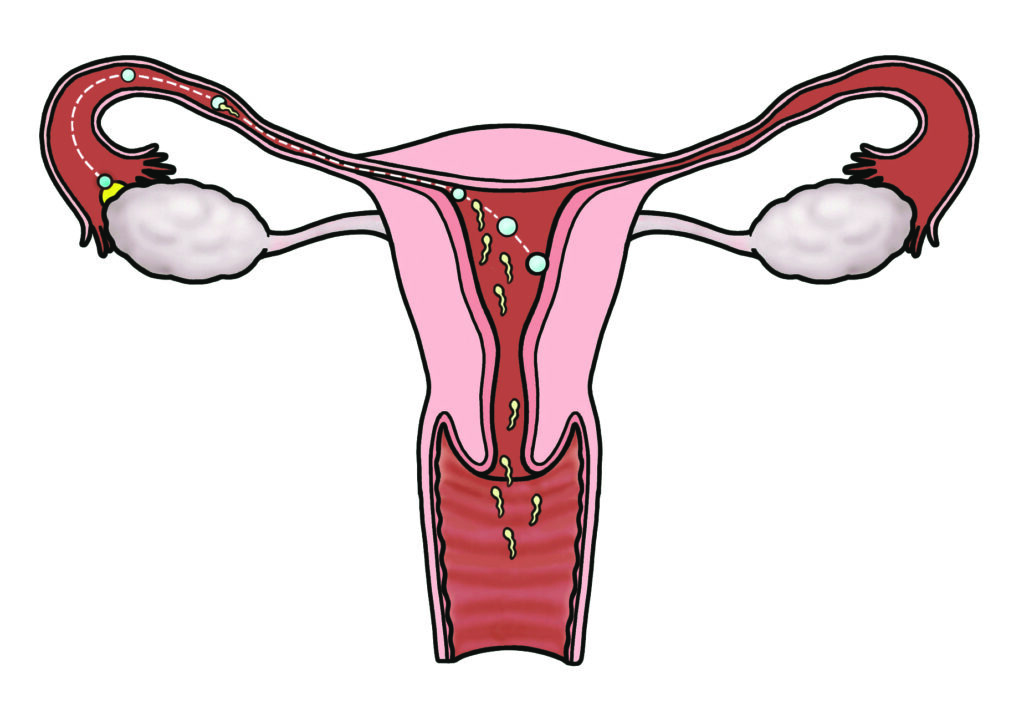
Once an egg is released (ovulated) it is picked up by the fallopian tube and carried towards the womb. It meets the sperm in the tube and fertilisation happens here. The embryo (fertilised egg) then attaches to the endometrium (womb lining). The womb lining grows in response to increasing oestrogen in the body and following ovulation, progesterone helps the embryo to implant and grow into a baby.
What causes ovulation problems?
In some cases, ovulation does not happen naturally. It may be that it takes a lot longer to release an egg. This is often suspected if your menstrual period happens irregularly or does not happen at all. There are lots of reasons that you may not ovulate, some of the more common ones are:
Polycystic Ovary Syndrome (PCOS)
This is the most common cause for ovulation problems in the young. There can be a mixture of symptoms including irregular periods, acne and unwanted extra hair growth. The ovaries with PCOS can often have a very typical appearance on ultrasound.
For reasons that we still do not completely understand, some of the follicles that contain eggs get stuck in the natural process of turnover and form ‘cysts’ seen on ultrasound scanning. This in turn means an egg does not grow enough to be released.

More information about PCOS can be found in a separate booklet available on our website. See link below:
Pituitary problems
If the ‘master’ gland in the brain does not work properly, FSH and LH are not released at the right time. People who are overweight, underweight or exercise too much can have problems with their pituitary gland function. High levels of stress can also affect the pituitary gland. Some pituitary problems are referred to as hypogonadotropic hypogonadism (low hormone signals from the brain leading to low hormone responses from the ovaries).
Thyroid problems
The thyroid is a gland in your neck, which produces a hormone that is responsible for your metabolic rate (e.g. heart rate and body temperature). If you have too much or too little thyroid hormone, it can affect ovulation.
High prolactin level
Prolactin is another hormone produced by the pituitary gland. If too much prolactin is produced it can increase the hormone oestrogen and affect ovulation. Sometimes medications used for other conditions can cause extra prolactin to be released.
Premature ovarian insufficiency
Some people have fewer eggs in their ovaries or use the eggs up more quickly. As this happens the menstrual cycle can become irregular and eventually stop, meaning no more eggs are left in the ovaries to ovulate. Unfortunately, ovulation induction is unlikely to be very successful in this situation.
Ovulation Induction (OI)
Is the medical process of stimulating the ovaries to release an egg. It usually involves drugs (either tablets or injections) but can be done during surgery, provided there are no other fertility problems.
What tests will I have before starting?
Before starting any fertility treatment, you will have tests to try to work out why you are having problems getting pregnant. If you have irregular periods or no periods the important tests will include:
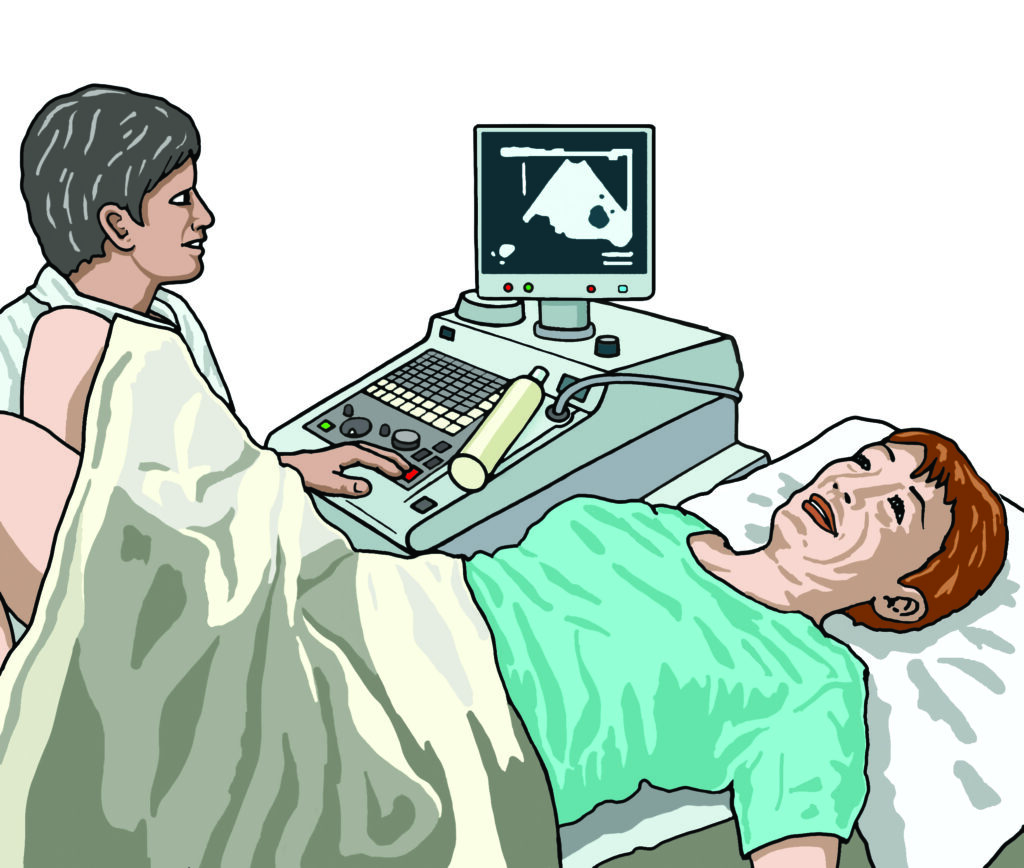
Ultrasound scan
To check that the ovaries look healthy and to give an estimate of how many eggs they contain.
Tubal patency test
To check that the fallopian tubes are open to allow the egg and sperm to meet. There are different ways of doing this dependant on your medical history:
- Hysterosalpingogram (HSG) using x-rays.
- Hystero-salpingo contrast sonohysterography (HyCoSy) using ultrasound.
- Laparoscopy during a surgical operation under general anaesthetic.
Your doctor will advise you which option (s) are most suitable for you and explain why.
Sperm test
If you have a male partner, a sperm test will be needed to check that there are healthy sperm being produced.
Hormonal blood test
We can test for your pituitary (FSH / LH / Prolactin), ovarian (oestrogen /testosterone) and thyroid hormones, which will help to direct treatment.
What are the options for ovulation induction treatments?
If you do not have a regular period, you may need to take a tablet that makes you bleed before starting a treatment cycle (Provera). This is called a withdrawal bleed and allows OI to start.
Clomifene Citrate / Clomid (CC)
Clomifene works by reducing the effect of oestrogen on a part of the brain known as the hypothalamus. This improves the release of FSH and LH from the pituitary gland, helping an egg to grow in the ovary and ovulation to occur.
A tablet is taken daily from the second day of your period for 5 days. In your first treatment cycle, an ultrasound will take place between 8-10 days after starting CC. This is to make sure that you are responding to the tablets and that there are not
too many eggs preparing to be released.
Further scans and / or blood tests will be organised according to the findings. At least one more scan and blood test are organised to confirm ovulation (usually a week after when we think ovulation should have occurred).
If you respond well to the tablets you will be prescribed enough to take over three cycles at home without further scan monitoring. You should keep a record of when your periods come to count the number of days in each cycle. If you have a positive pregnancy test, you should let Leeds Fertility know and we will arrange a pregnancy scan, hopefully to confirm that all is well. If you do not conceive within three months, an out-patient review with a doctor is needed to decide if more CC can be given or if a change in treatment is indicated. Clomifene is usually only given for 6 months (6 ‘cycles’). We recommend that you have regular sexual intercourse, 2-3 times a week before, during and after ovulation, when we have confirmed that the drug is working correctly.
Side effects of CC:
Fairly common:
- Headaches.
- Hot flushing.
- Nausea.
- Breast tenderness.
Occasionally:
- The womb lining (endometrium) may not thicken properly which is not helpful for a developing pregnancy. If this occurs we may consider other treatment.
Rarely:
- Disturbance in vision: If this happens to you, please stop CC immediately and contact the nursing team at Leeds Fertility for advice. See ‘Contact us’ section for details.
Letrozole
Letrozole works in a similar way to CC, by reducing the strength of the oestrogen signal in the brain. This allows more FSH and LH to be produced from the pituitary gland to help an egg grow in the ovary. It does not affect the endometrium in the same way as CC.
Although Letrozole is not licensed for use in ovulation induction, it is being used more and more in fertility clinics. It is taken in tablet form from the second day of your period for 5 days. Ultrasound monitoring is done to make sure the drug is working.
This drug may be used if you do not respond to clomifene or has produced too many growing eggs with CC. The side-effects are similar to CC.
Gonadotrophins
The hormones FSH and LH which are produced by the brain to instruct the ovary to get an egg ready each month can be given directly, by daily injection. These are known as gonadotrophins.

There are many different brands available but they all work in the same way.
An ultrasound scan at the start of your period will make sure that there are no ovarian cysts and that the lining of the womb is ready to start treatment. You will be taught how to give yourself daily gonadotrophin injections, usually into your tummy or upper leg. You will need to have a few scans through the treatment cycle to monitor when a follicle (a sac that contains an egg) starts to grow in your ovary.
Although it varies from person to person it usually takes two weeks of injections until the egg is ready to be released. When a follicle is big enough, you will be instructed to take a second injection (trigger injection), which contains the hormone human chorionic gonadotrophin (hCG) to help the egg to release. You will then be advised to have regular intercourse 2-3 times a week.
You may have timed insemination with a specially prepared sperm sample from the partner / donor.
This is called intra-uterine insemination (IUI).
Please note
If too many follicles grow at the same time you will be at risk of getting pregnant with twins, triplets or sometimes more.
It is very important that you follow our advice to stop the injections and avoid unprotected sex until your next period.
Some women may develop ovarian hyperstimulation syndrome with this treatment. This can be uncomfortable and can lead to complications.
Side-effects of gonadotrophin OI:
Most people taking gonadotrophins do not feel unwell.
Fairly common:
- Over-stimulation (producing 3 or 4 eggs at once) is fairly common but rarely dangerous. It is more frustrating that an attempt to conceive has to be missed that cycle.
Rare:
- Ovarian hyperstimulation syndrome (OHSS).
Ovarian hyperstimulation syndrome can develop when too many follicles (sacs containing the eggs) grow at the same time. The main symptoms are:
– Swelling and discomfort in the tummy due to enlarged ovaries and retained fluid.
– Sickness and loss of appetite.
– Diarrhoea.
Usually it will settle by itself with simple pain relief, hydration and rest. Sometimes other measures are needed.
Please see our separate information booklet about OHSS if necessary. A link to this leaflet is provided below:
Ovarian Drilling
Ovarian ‘drilling’ can be done during a laparoscopy key-hole operation, under general anaesthetic (while you are ‘asleep’). Small areas of the ovary surface are cauterised (treated with heat / charred) and this has been found to help ovulation. This is usually only offered if you are having an operation anyway to investigate your fertility or other gynaecological symptom. You may find that your menstrual cycle becomes regular after the operation and the positive effects of surgery may last up to 6 months. Regular intercourse is recommended during this time.
There are risks when you have a laparoscopy operation, although serious problems are rare. Separate information about the procedure is available. Please see our Diagnostic Laparoscopy patient information leaflet. A link to this leaflet is below:
The more serious risks include injury to your bowel, bladder or blood vessels inside your body. There can be some scarring inside whenever you have an operation. Due to the risks, we usually only offer this treatment if you need an operation anyway or if you haven’t responded to any of the treatments discussed above.
What are the risks of ovulation induction?
There are risks when drugs are used to stimulate the ovaries. These can be serious and need hospital admission.
If you are ever worried about symptoms you are experiencing you should always contact your monitoring fertility clinic, who will advise you about what to do.
Ovarian Hyperstimulation Syndrome (OHSS)
- Please see our separate information about OHSS.
Multiple pregnancy
If more than one follicle grows there is an increased risk of multiple pregnancy. This is usually twins (two babies) but can be triplets (three babies) or more. Multiple pregnancy is associated with more risks both for the mother and the babies including:
- Miscarriage.
- Prematurity (baby born too early risking disability).
- High blood pressure and preeclampsia in the mother.
- Diabetes in the mother which affects both mother and babies.
Due to these risks, our aim is to produce one healthy baby at a time. This may mean that an OI treatment is abandoned if too many eggs are growing in your ovaries at the same time.
A lower dose of treatment may be needed next time, or a different treatment altogether.
Ovarian cysts
Ovarian cysts can happen if a follicle grows and either doesn’t release an egg or doesn’t shrink after ovulation. This type of cyst rarely needs any treatment and will usually disappear on its own over a couple of months. You can sometimes experience pain, particularly if the cyst ‘pops’. This is usually managed with simple painkillers such as paracetamol or ibuprofen. The next cycle of treatment may need to be delayed to wait for the cyst to disappear naturally before a new follicle is stimulated to grow.
Miscarriage
About 1 in 4 pregnancies ends in miscarriage whether they are naturally conceived or with assistance. You are not at an increased risk of miscarriage by using ovulation induction.
Ectopic pregnancy
Any pregnancy can attach (implant) and start to grow in the wrong place. The fallopian tube is the most common area. This type of pregnancy can be dangerous and needs to be managed by a doctor. Getting pregnant with ovulation induction treatment does not increase the risk of ectopic pregnancy compared with unassisted pregnancy.
Ovarian cancer
It has been suggested in the past that ovulation induction may lead to ovarian cancer. Lots of research has looked into this suggested risk and the results are reassuring. To prevent any theoretical, if a pregnancy hasn’t happened within the first 6 months, we will usually change the recommended treatment to try to improve your chance of having a baby. It is not recommended to take more than 12 treatment cycles of CC.
What is intra-uterine insemination?
Sometimes OI is combined with intra-uterine insemination. This is when sperm is put into the womb when ovulation has happened. Ovulation is usually detected by testing your urine with an ovulation LH-testing kit, purchased from a chemist or large supermarket. You will call your fertility clinic when your kit gives a positive signal for ovulation and they will organise the insemination to happen, usually on the following day. The sperm is prepared on the day, to ensure that only the healthy active sperm are used. The procedure is similar to the examination done for taking a smear. It is not painful. A small tube (catheter) will be inserted through your cervix (neck of the womb) and the sperm will be injected inside. The procedure takes around 10 minutes. You will be able to carry on with normal day-to-day activities straight after the treatment. If a period doesn’t start at your usual time or 2 weeks after the IUI, you should do a pregnancy test. If it is positive an ultrasound will be organised for you when you are 7 weeks pregnant.
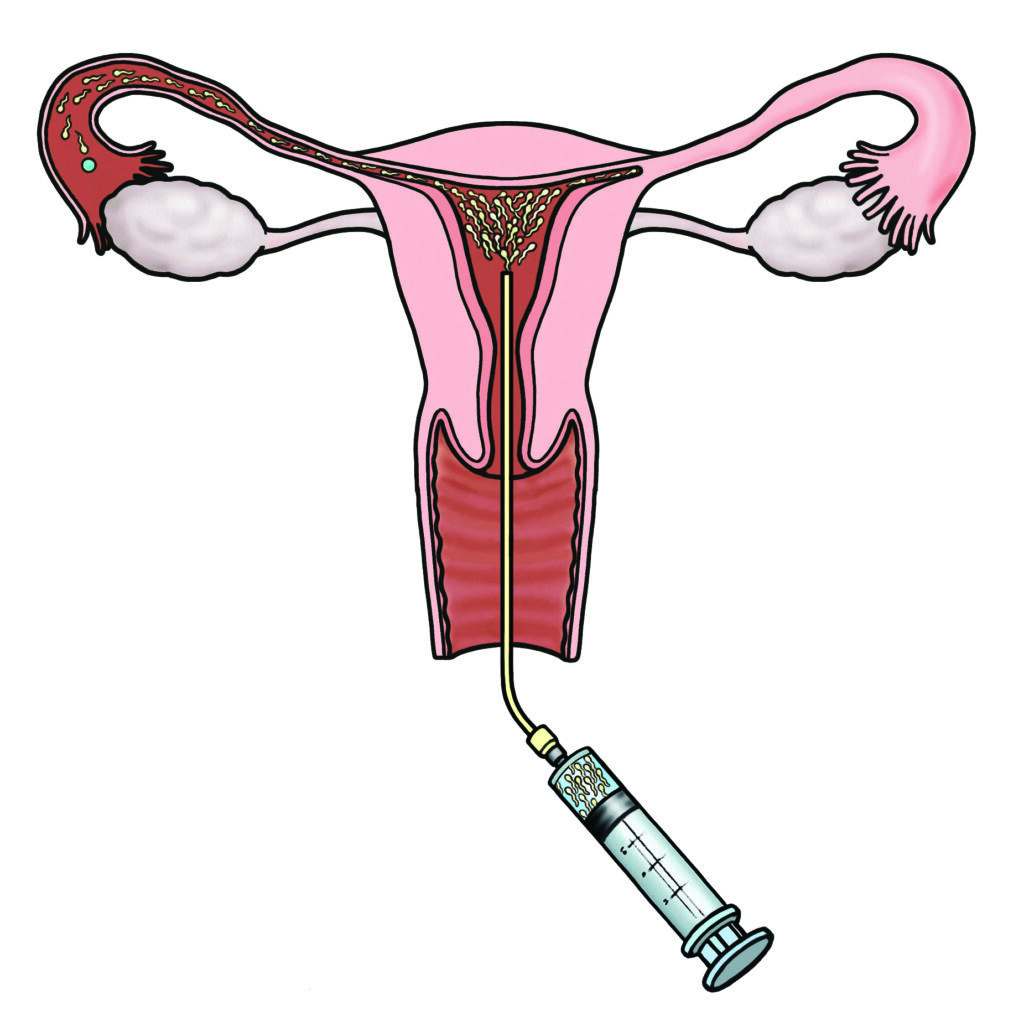
For couples who have regular intercourse and a normal sperm test, IUI is unlikely to offer any further advantage. For those couples who need donor sperm or have difficulties having intercourse, IUI can be very successful.
What are the success rates of ovulation induction?
The time in the cycle when it is possible to get pregnant is limited and is called the ‘fertile window’. This is mainly the week around ovulation. To ensure sperm is available when an egg is released the general advice is to have sex regularly throughout the month, but especially before ovulation.
This is really important, if you are taking tablets at home without ultrasound monitoring or have had ovarian drilling to ensure the best chance of pregnancy. If you are having ultrasound monitoring within the clinic, you will be advised when to have intercourse.
Days in the cycle with the highest chance of getting pregnant
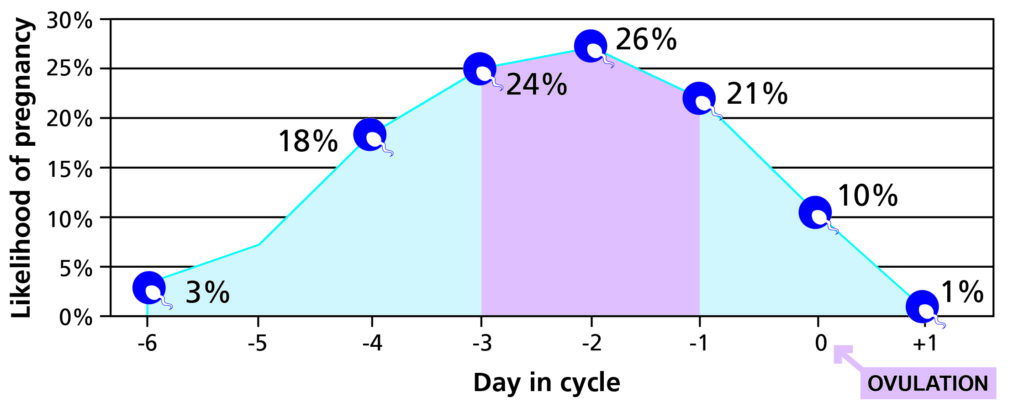
Image adapted from https://britishfertilitysociety.org.uk/fei/when-are-women-men-most-fertile
The success rates for these treatments depend on the underlying cause of your ovulation problems, age and general health including your weight. Ovulation induction may restore normal pregnancy rates of 20-25% per cycle. The majority of patients (60%) of patients will conceive within the first 3 months.
The success rates for intra-uterine insemination are ~12%. For those who are under 35 years of age it is 14%. As you get older the chance of success goes down.
What can I do to prepare for healthy pregnancy and boost my chances of success?

- Stop smoking completely.
- Reduce alcohol intake to a minimum for both you and your (male) partner. No safe limit has been identified for women so no alcohol consumption is advised. Men should ideally restrict alcohol intake to 3 to 4 units per week.
- You should restrict your caffeine intake as this has been shown to lower IVF success rates.
- You should have been vaccinated twice against German measles (rubella) or have confirmed immunity.
- You should have an up to date, normal cervical smear test.
- You should be taking folic acid (vitamin B) supplement at 400 micrograms daily before and during treatment, and for at least the first three months of pregnancy. Vitamin D 10 micrograms should be taken throughout. Over-the-counter multivitamins for pregnancy should contain the necessary ingredients.
- Both partners should aim for normal body weight for their height. You in particular should aim for a body mass index ideally under 25kg/m2, and absolutely under 30kg/m2 to access NHS-funding. Treatment is less successful and more risky at heavier weights. Pregnancy is also less healthy with a higher risk of blood pressure problems and diabetes if your BMI is high.
- A healthy, varied diet and regular physical exercise are helpful for overall health, weight management and stress reduction. Please see the website for more information on preparing for pregnancy.
Counselling
We recognise that struggling to conceive can be upsetting. We aim to provide supportive care for both partners through this process, regardless of the outcome.
Specialist counsellors provide support in dealing with the social and emotional aspects of fertility problems and help to find ways to cope with the on-going situation.
Counselling is accessible through your fertility clinic. Please contact them directly.
Other resources
Glossary
- Androgen: A term to include steroid hormones that promote features often related to the male.
- Anti Mullerian hormone: Is produced by the growing follicles in the ovary and is often very high in women with PCO and PCOS.
- Clomiphene Citrate: An anti-oestrogen oral medication used to help ovulation.
- Diabetes: A condition of abnormally high blood sugar levels related to ineffective insulin
- Eggs: A woman’s lifetime supply of eggs is present in the ovary at birth. They reduce in number and quality with time. They pass on the half of the genetic instructions to the embryo/baby.
- Endometrium: The lining of the womb.
- Fertilisation: Fertilisation is when the genetic material from the egg and sperm combine to create a new and unique cell which may go on to develop into an embryo and then a baby.
- Follicle: An egg-bearing sac in the ovary
- FSH: Follicle Stimulating Hormone causes the eggs to mature in the ovary.
- Gonadotrophins: Hormones produced naturally by the pituitary gland to stimulate the ovary to produce and release eggs e.g. FSH, LH. These drugs are produced as medicines to over-stimulate the ovary during IVF / egg freezing to get lots of eggs ready at once e.g. Meriofert, Menopur, Gonal F.
- Hirsutism: The medical description of excessive hair growth.
- Intra-uterine insemination: Sperm is placed inside the womb following ovulation.
- Letrozole: A medication used to help ovulation.
- Oestrogen: This hormone is naturally produced by the follicle in the ovary as the egg is growing. Its main job is to thicken the lining of the womb for a pregnancy to implant.
- Ovary: Stores all the woman’s eggs for her whole life and produces hormones.
- Ovulation: When an egg is released from the surface of the ovary and pregnancy is possible; without pregnancy a period follows in 2 weeks; the absence of a period signals pregnancy has occurred or ovulation did not occur.
- Pituitary gland: In the head, behind the nose, the master gland which produces many hormones including those that control the ovary and testis.
- Polycystic Ovary: An ovary that has at least 12 small ‘cysts’ (follicles) on ultrasound scan.
- Polycystic Ovary Syndrome: A combination of symptoms that may include irregular periods, androgenic symptoms (acne or unwanted hair growth and ultrasound features of a polycystic ovary).
- Progesterone: The hormone produced by the ovary after ovulation to prepare the womb lining for implantation of a fertilised egg and the start of pregnancy.
- Progestogen: A synthetic form of progesterone found in all hormonal contraceptives (pills, injections, implant, coil).
- Prolactin: A hormone produced by the pituitary gland which helps with breast milk production. Sometimes it can be made in large amounts by too many active cells and one side effect is to make the periods disappear.
- Sperm: The sperm develop in testes and continue to do so throughout adult life. They do not suffer the same deterioration with age as eggs, as they are constantly being replaced. They pass on half of the genetic instructions to the embryo / baby.
- Testosterone: The hormone mainly produced from the ovaries that may give unwanted symptoms e.g. facial hair, acne and hair thinning.
Contact us
Please note
For urgent questions whilst in treatment, please contact your fertility clinic provider.
Other leaflets
- LN002313. Polycystic Ovary Syndrome leaflet.
- LN003437. Ovarian Hyperstimulation Syndrome (OHSS) leaflet.
- LN004469. Diagnostic Laparoscopy and hysteroscopy under general anaesthetic leaflet.