A gene change has been found to run in your family. These gene changes lead to an increased risk of breast cancer and sometimes, other cancers such as ovarian and prostate.
Introduction
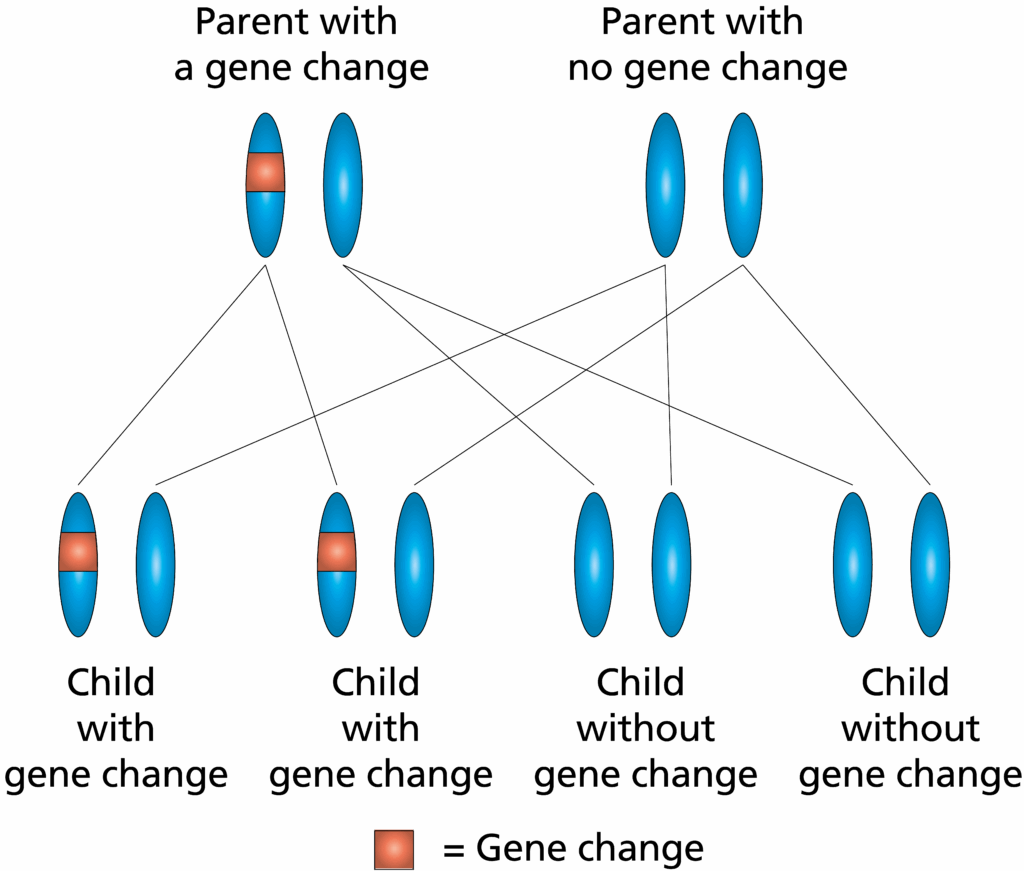
We all have more than 20,000 genes. Each gene is an instruction within our body. Changes in that instruction can affect how it works. Some of these genes are important in protecting us from cancer. We have two copies of each of these genes; one from each biological parent. A change in just one of those two copies of the gene will increase the risk of developing certain cancers in that person.
When we have our children we pass only one copy of each gene on, with the other copy coming from our partner. If a parent has a gene change, there is a 50% chance for each of their children of inheriting the gene change and a 50% chance of not inheriting it. These gene changes can be inherited by males and females. There is no way at present to reverse the gene change but there is screening and surgery available to help protect against the chance of cancer developing or detect it early.
Not everyone who has a gene change will develop cancer.
The Leeds Teaching Hospitals NHS Trust
Options for people with a gene change linked with breast and other cancers
In women
A combination of MRI scans and mammography is used to screen for breast cancer, depending on age and breast tissue density. The age at which screening starts is based on the type of genetic change in your family. This usually means starting breast screening at age 30 or 40.
Calculating cancer risk levels for each person
For every person, even with the same gene change, the levels of cancer risk vary. This depends on a person’s age, family history and a variety of lifestyle / environmental factors such as exposure to hormones like oestrogen.
The levels of cancer risk can be different for transgender men and women, depending on any surgery the person has had and their exposure to hormones.
The health professional looking after you can help you to understand the risk levels for you as an individual.
Back to topBreast and chest awareness
No breast screening method detects all breast cancers. It is important to understand that breast screening cannot prevent cancer and that cancer can develop in between the screening appointments.
Regular self-examination and breast / chest awareness is very important. If new breast symptoms develop, including any lump, changes in the skin or nipple, rash or discharge, please arrange a check-up with your GP without delay.
Mammography – benefits and disadvantages
A mammogram is a low-dose x-ray of the breast.
MRI screening
MRI (magnetic resonance imaging) scans use magnetism rather than x-rays to look at the breast tissue. MRI does not increase the risk of breast cancer. Research shows MRI detects more abnormalities in the breast tissue than mammograms, although they will not all be cancer. A needle biopsy will usually be required if any abnormality is detected, to clarify whether there is cancer present or not. MRI screening is usually only suggested for younger women or women with very dense breasts.
Risk-reducing mastectomy
Bilateral risk-reducing (or ‘prophylactic’) mastectomy is the surgical removal of the breast tissue, from both breasts, to reduce the risk of breast cancer developing. This option is available where the risk of developing breast cancer is calculated as being more than 30% over a person’s lifetime so it is not applicable to all people with a gene change. This operation reduces the risk of breast cancer by over 90%. It is a major operation, which can have surgical complications and emotional effects. Breast reconstruction is offered as routine with risk-reducing surgery. There are various different options for breast reconstruction, which depend on each individual’s body size and shape. The Breast Surgical teams are happy to discuss this with anyone considering this option.
Other options
There have been guidelines published which suggest that some women who are at increased risk of breast cancer may be considered for treatment with a tablet called Tamoxifen, or a similar drug, to reduce the risks of developing breast cancer. There is a separate information leaflet about this topic. It is not suitable for all women.
Back to topOvarian cancer
Symptoms of ovarian cancer can be difficult to notice. They include persistent abdominal (tummy) pain, bloating, difficulty eating, feeling full very quickly and the need to pass urine more frequently. Research is on-going to determine if any screening tests may be helpful but currently there is no nationally recommended screening for ovarian cancer. The chances of developing ovarian cancer can be reduced to less than 3% by surgical removal of the fallopian tubes and ovaries (prophylactic bilateral salpingo-oophorectomy (BSO). There is a rare cancer affecting the peritoneum (lining of the abdomen) which is not prevented by this surgery. Not all gene changes are linked to an increased risk of ovarian cancer and so is not applicable to all people with a gene change.
For some, having a BSO before the age of natural menopause may also reduce the risk of breast cancer.
BSO can often be done via keyhole surgery. The age at which it is offered varies depending on the gene change and family history. It would not usually be considered before the age of 35 and until it was felt that the individual’s family was complete. BSO will cause an immediate menopause if the natural menopause has not already begun. Removal of the ovaries can increase the risk of other problems, including osteoporosis (thinning of the bones). Hormone replacement therapy (HRT) is usually advised for a limited period after BSO, up to the age of around 50, in a woman who has not been affected with breast cancer previously.
Prostate cancer
Depending on the gene change identified, it may be appropriate for people at increased risk of prostate cancer to have a regular blood test. This blood test checks the level of prostate specific antigen (PSA). Your genetic counsellor or doctor will advise whether this is relevant on an individual basis.
Cancer Research UK has a useful information page on the blood test, PSA (Prostate-specific Antigen), which may be raised if a cancer of the prostate is developing.
Cancer Research UK Back to topGenetic testing
If a specific gene change has been found in a family member, others in the family can have a ‘predictive’ genetic test. This allows them to find out whether they have inherited it or not. This testing is usually only offered to adults. There is a one in two chance of inheriting a gene change from a parent who has it. If it has not been inherited, then the chances of developing the cancers discussed above are not increased and screening or surgery to reduce the risk is not needed. Someone who has not inherited the gene change cannot pass it on to their own children.
If the gene change has been inherited, then the options described above could be considered, where appropriate.
Genetic testing and insurance
There is currently an Association of British Insurers (ABI) code on genetic testing and insurance. This means that you do not have to tell the insurance company about the result of a predictive genetic test when taking out life insurance or critical illness cover. You do need to tell them about your family history, if asked. You can tell them your result if you do not have the gene change as this should help reduce the premiums. You can read more on the ABI website.
Family planning options
Most people with a gene change will have their children as usual. Some people with a gene change want to ensure that it is not passed on to the next generation. They may consider the possibility of Pre-implantation Genetic Testing (PGT). This incorporates In-Vitro Fertilisation (IVF) with genetic testing, aiming to implant an embryo without a gene change. It is a complicated process with a success rate of about one in three per cycle of IVF. In some cases, it is also possible to offer genetic testing in a pregnancy that has been conceived naturally. Further information about these options is available on request.
Other family members
This information may be relevant to other adult members of your family. If they wish to be seen in the Genetics Clinic to discuss the gene change that has been identified in the family, they can be referred by their GP quoting the family reference (PED) number given at the top of any letters we send you.
Back to topFurther information
You may find the following websites helpful: