This booklet has been written to answer some of the questions you may have about vulval surgery.
You will be given a separate leaflet called ‘Gynaecological Oncology Surgery – Enhanced Recovery Programme’ which will explain about what to expect when you come in for your surgery and advice for recovery at home.
If you have recently been diagnosed with cancer of the vulva you may find that you are experiencing a wide range of emotions. These can include fear, anger, denial, low mood and anxiety. Reactions differ from one person to another and there is no right or wrong way to feel. Whatever you may be feeling at present, try talking about it with someone who can help; such as your consultant, gynaecology specialist nurse or GP. They will listen to you and answer any questions that you may have. They can also put you in touch with other professionals or support organisations if you wish. Some useful contact numbers are listed at the back of this booklet.
On this page
- What is vulval surgery and why is it necessary?
- Types of surgery
- Removing the skin covering the vulva (for VIN)
- Wide local excision
- Removing part of the vulva
- Removing the whole vulva
- Sentinel lymph node biopsy
- What are the risks of vulval surgery?
- Will I have a scar?
- Is there anything I should do to prepare for the operation?
- Vulval hygiene
- General advice after surgery
- Is it normal to feel weepy or depressed after my operation?
- When can I have sex?
- Will I need to visit the hospital again after my operation?
- Additional information
- Useful Numbers
- Website
- Contacts
- Local Support Services
- National Information and Support
What is vulval surgery and why is it necessary?
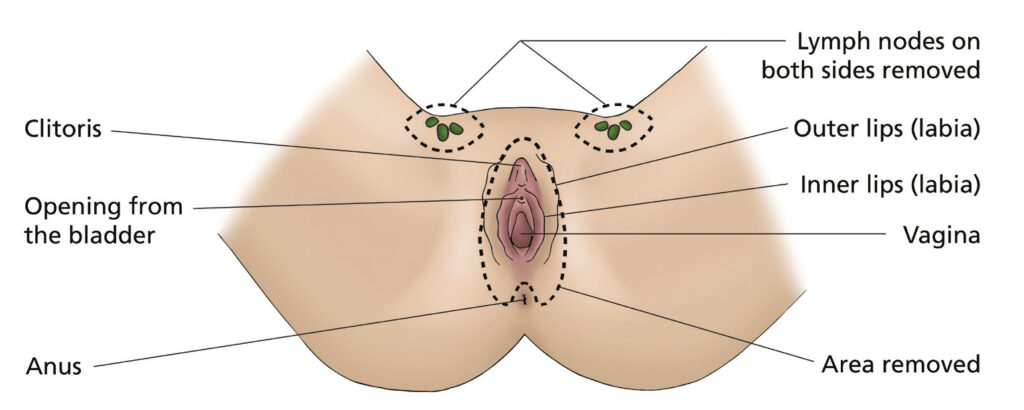
Women with cancer of the vulva may need to undergo surgery to remove either some or all of the tissues in this area (see diagram below).
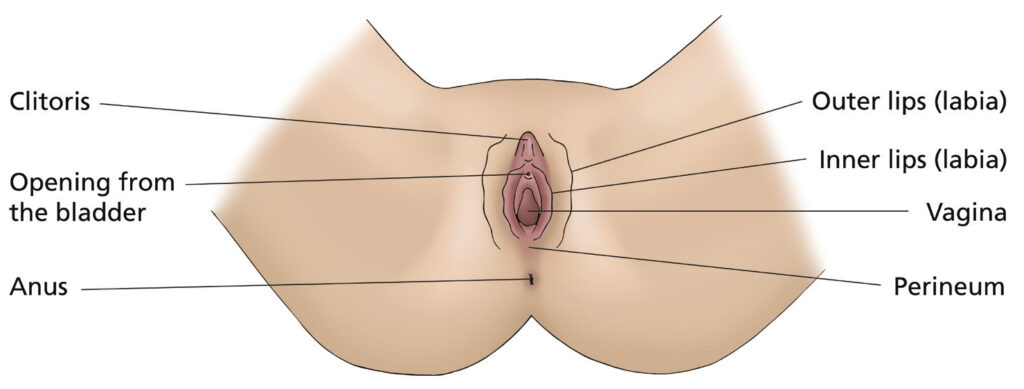
The type of surgery will depend upon the size and site of your cancer, your general health and any symptoms you may have such as discomfort, pain, burning or itching.
The aim of the operation is to remove all of the cancer, at the same time trying to preserve as much vulval tissue as possible. Surgery for this disease in its early stages is usually very successful. However, if the cancer has spread, radiotherapy to the area may be recommended.
Types of surgery
Removing the skin covering the vulva (for VIN)
This operation is called a skinning vulvectomy and is used to treat vulval intraepithelial neoplasia (VIN). VIN is a pre-malignant skin condition where the cells on the surface of the vulva are abnormal. It is not cancer but has a small risk of developing into cancer over many years. Because the affected cells are only on the vulval surface, it is possible to take away only the skin and leave the healthy tissue underneath. You will usually be able to go home on either the same day or the day after your operation.
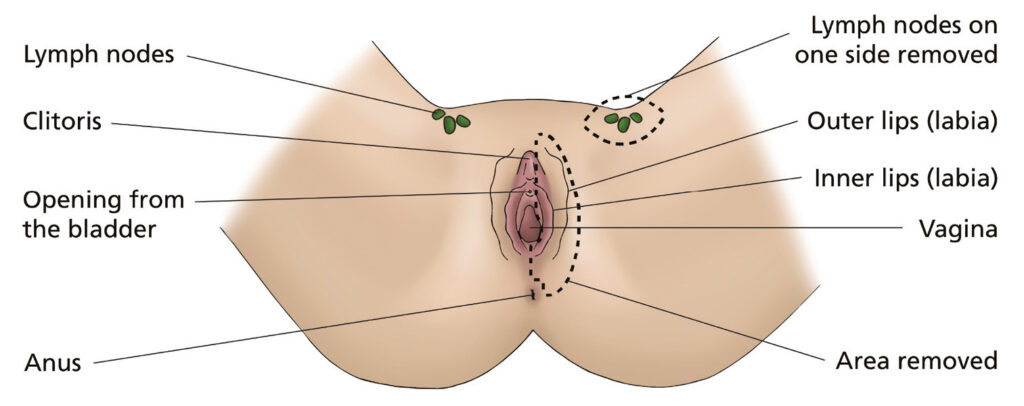
Wide local excision
This operation is usually recommended if the cancer is quite small. The area containing the cancer is removed, along with a border of healthy tissue around it. With this operation, you may also have lymph nodes removed from the groin, on the same side as the cancer (lymph node dissection). You will be able to go home one to three days after your operation depending on the extent of your surgery.
Removing part of the vulva
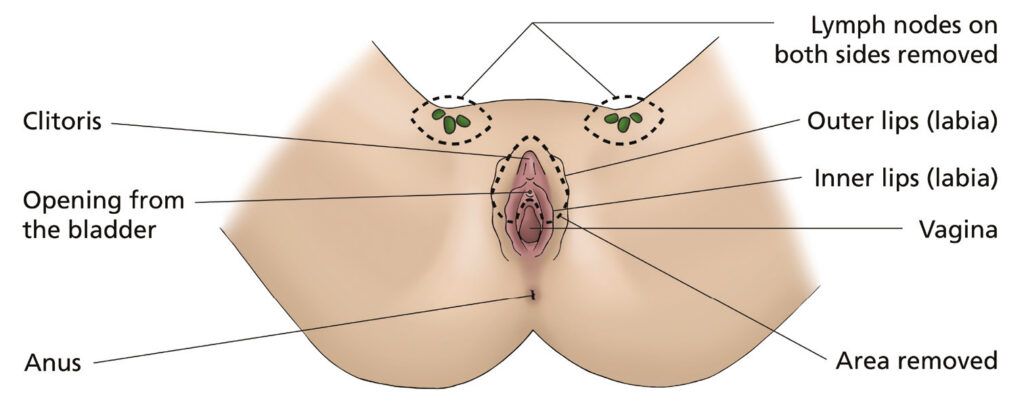
This operation is called a partial vulvectomy. This may involve having just the inner or outer labia removed or the labia may be removed from one side only. How the operation is done and whether the lymph nodes are removed (lymph node dissection) from one or both sides of the groin will depend on where the cancer is. If lymph nodes are removed from both sides of the groin then this is called a triple incision vulvectomy, as there is one incision to remove part of the vulva and two more – one on each side- to remove the lymph nodes. You will have either one or two wound drains placed into your groin, so that any blood or fluid that collects in the area can drain away safely. You will go home with these drains in and return to the out-patient clinic about two to three weeks later where they will usually be removed. You should be able to go home five to ten days after your operation.
Types of partial vulvectomy
Hemi-vulvectomy
Anterior vulvectomy
Posterior vulvectomy
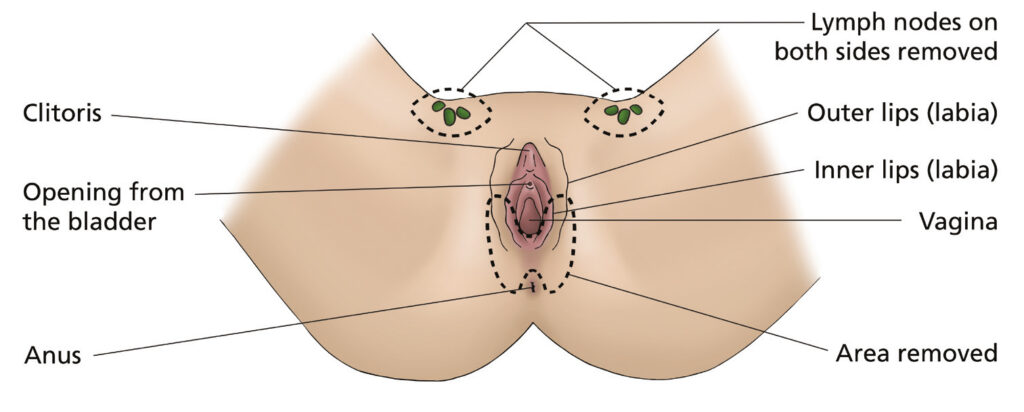
Removing the whole vulva
This operation is called a radical vulvectomy. It involves having the entire vulva removed, including the inner and outer labia and the clitoris. The lymph nodes are usually removed from both sides of the groin (lymph node dissection). The operation is often known as a triple incision vulvectomy as there is one incision to remove the vulva and two more – one on each side – to remove your lymph nodes. You will usually have two wound drains placed into your groin, so that any blood or fluid that collects in the area can drain away safely. You will go home with these drains in and return to the out-patient clinic two to three weeks later where they will usually be removed. You should be able to go home five to ten days after your operation although some women may need to stay on the ward a little longer.
Radical vulvectomy
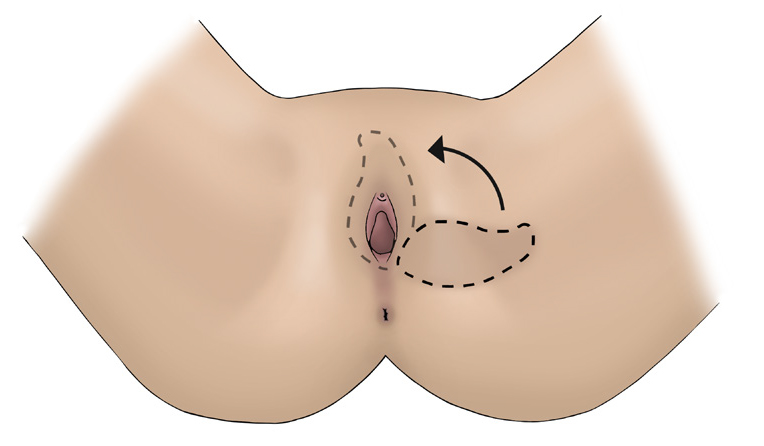
Some women may need to have surgery to reconstruct their vulva using a skin flap.
A skin flap is made from a piece of skin close to the vulva that is moved (rotated) onto the vulval area to cover the wound. This would usually be done at the same time as the
operation to remove the cancer.
Sentinel lymph node biopsy
What is a sentinel lymph node?
A sentinel lymph node is the first lymph node that vulval cancer cells usually spread to. In some cancers, this lymph node is present on both sides of the groin.
Identifying and removing the sentinel lymph node and checking for cancer spread helps us to avoid the need for removal of all the lymph nodes from the groin in women who have negative sentinel nodes. This reduces the risk of long-term complications like lymphoedema and cellulitis.
Is this procedure safe?
A large multi-national study (GROINSS-V study) showed that, in early-stage vulvar cancer, patients with a negative sentinel node had a low chance of cancer recurrence in the groin with excellent survival. The treatment-related side-effects were minimal and the technique was found to be safe and accurate. Recent guidelines from the Royal College of Obstetricians and Gynaecologists recommend the use of sentinel lymph node biopsy in clinical practice for early stage vulval cancer.
Why would I be offered this procedure?
Studies have shown that in patients with small vulval cancers with no enlarged lymph nodes on scan, the sentinel lymph node biopsy is a safe alternative procedure to removing all the groin lymph nodes, with minimal side-effects. Your doctor will discuss this procedure following the cancer team meeting if they feel it is safe to perform this in your case.
How is the sentinel node identified and removed?
You will have a small injection of a harmless radioactive marker into the skin next to the cancer on the morning of the operation. This will happen in the Nuclear Medicine department. A series of images will be taken using a gamma camera for 30 minutes after the injection. Further images at 2.5 hours after the injection may be needed.
If the sentinel lymph node is not identified using the gamma camera, a special type of CT scan called SPECT-CT may need to be performed to locate the sentinel node.
Later that day you will have your operation as planned. Whilst you are asleep we will inject some blue dye around the cancer which will also help us to locate the sentinel nodes. We will then identify and remove only the sentinel lymph nodes(s) from one or both groins. The nodes(s) will be sent away for detailed assessment by the pathologist. During the operation we will also remove the cancer from the vulval area if appropriate.
You will usually be able to go home within a few days depending on the extent of vulval surgery.
What happens if the sentinel node is not found?
If the sentinel node is not found, then all the groin lymph nodes will need to be removed from the side where the node has not been identified. The chance of not finding the sentinel lymph node is less than 5%.
What might the results of the sentinel nodes show?
The results are available (usually within three weeks) after the operation.
- If the sentinel nodes are free from cancer you will not require further surgery. We will simply follow you up closely with visits to the clinic every three months for the next two years.
- If the sentinel nodes are shown to contain any cancer spread, treatment will be continued by surgical removal of all the remaining lymph nodes of the groin(s) in a second operation.
- Further treatment with radiotherapy may be required after removal of all the groin lymph nodes depending on the results.
What are the alternatives for treatment?
The alternative to sentinel node dissection is to remove all the glands from one or both groins (inguinofemoral lymphadenectomy). Patients with disease identified in more than one gland will then require radiotherapy or a combination of chemotherapy and radiotherapy.
Whilst these treatments are undoubtedly effective, they are associated with significant complications. These complications are greatest for those patients with spread of disease to the groins who typically require both radical surgery and chemoradiation/radiation.
What are the side effects?
Your urine will turn green-blue for the first day following your surgery because of the blue dye. The dose of radioactive marker is very small (~0.4 mSv). This is approximately the same as the amount of background radiation from the environment that you are exposed to over a period of 2-3 months.
There is a rare chance of an allergic reaction or anaphylaxis to the blue dye. If this occurs, this is usually dealt with effectively as you are already under general anaesthesia.
If the sentinel node is positive, then you will need a second operation at a later date to have the remaining nodes removed.
What are the benefits of having this procedure?
The sentinel node procedure is associated with a much lower rate of complications.
Unfortunately the standard operation of removing all the nodes from the groin is associated with significant and frequent complications. These complications include problems with the wound (such as infection or breakdown – 30-40% of patients), blood clots and long-term swelling of the legs (lymphoedema – 10-70% of patients). The hospital stay after conventional surgery is long, typically 4-7 days.
The sentinel node operation is quicker than the standard operation and the hospital stay is typically less than three days. Much less tissue is removed from the groins and the wounds are therefore stronger, with less risk of breakdown.
We would also expect there to be a reduced risk of clots following the sentinel gland operation. The evidence from removing sentinel nodes for other cancers (such as breast cancer) and our early experience with vulval cancer suggests that swelling of the leg will be less common following the sentinel node procedure. If swelling does develop it is likely to be much less severe.
Table 1. Benefits of sentinel node procedure as compared to standard groin node dissection.
| Standard groin node removal | Sentinel node operation | |
| Length of operation (to groin) | 45 minutes | 10-20 minutes |
| Length of hospital stay | 4-7 days | < 3 days |
| Wound infection/breakdown (groin) | ~30-40% | 11% |
| Lymphoedema | 10-70% | 5% |
| Recurrence risk / false negative rate | Typically 2-6% | ~2% |
| (estimates from literature) | 2-6 patients per 100 per annum | 2 patients per 100 per annum |
IMPORTANT
If you are breast-feeding, pregnant or planning to become pregnant, you should let your clinical team know. You should not become pregnant during treatment. If you become pregnant during treatment, you must inform your doctor or nurse immediately.
What are the risks of vulval surgery?
- Problems caused by having a general anaesthetic – for example you may feel sick afterwards. It is also possible to have an allergic reaction, although this is rare. Please tell your doctor about any allergies you have.
- Bleeding during or after the operation.
- Bruising around the wound site.
- Infection – this would be treated with antibiotics.
- Wound breakdown – this may be due to tightness in the surgical area where the tissue has been removed and the skin has been rejoined. If the wound is going to breakdown it normally happens within the first ten days after your operation. This may delay your discharge home from hospital. When you go home you may need a district nurse to visit you to continue caring for your wound until it has healed.
- A blood clot in the leg (deep vein thrombosis) which can sometimes lead to a blood clot in the lungs (pulmonary embolus) – moving around as soon as possible after your operation can help to prevent this. You will be given surgical stockings (known as TEDS) to wear and injections to thin the blood which both help to reduce the risk of blood clots. You may continue to have these injections for up to four weeks.
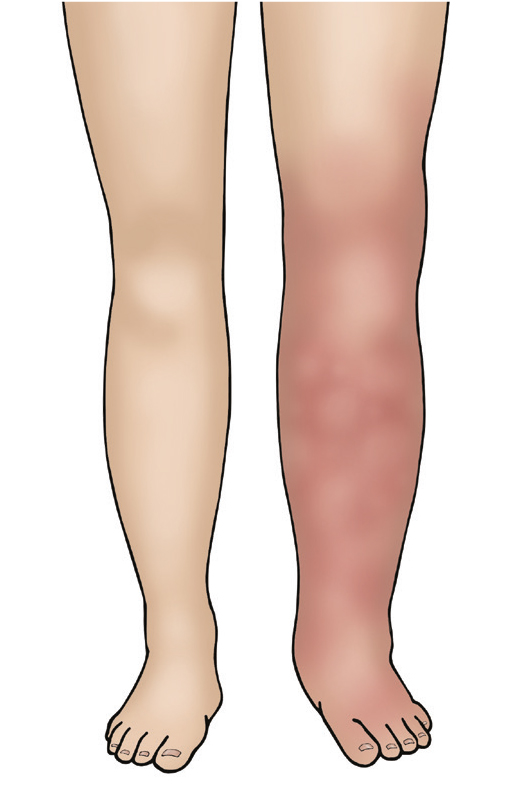
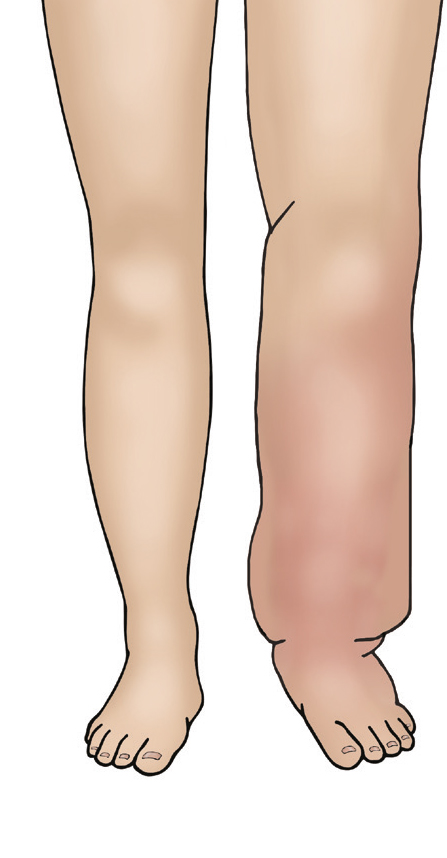
- Lymphoedema fluid circulates around your body draining through the lymph nodes. If your lymph nodes are removed from the groin area, either to stop the cancer spreading or because it already has, there is a greater risk of the lymphatic fluid not being able to drain away. The fluid may gather in one or both legs and/ or the genital area which will make them swell. This may happen months or years after your operation and is called lymphoedema. Lymphoedema can be managed and treated but there are things you can do to reduce the risk of it happening in the first place. There is a small section about lymphoedema on page 17. There is also a separate booklet specifically about lymphoedema that can give you more information. You can also discuss this further with your consultant surgeon or nurse specialist.
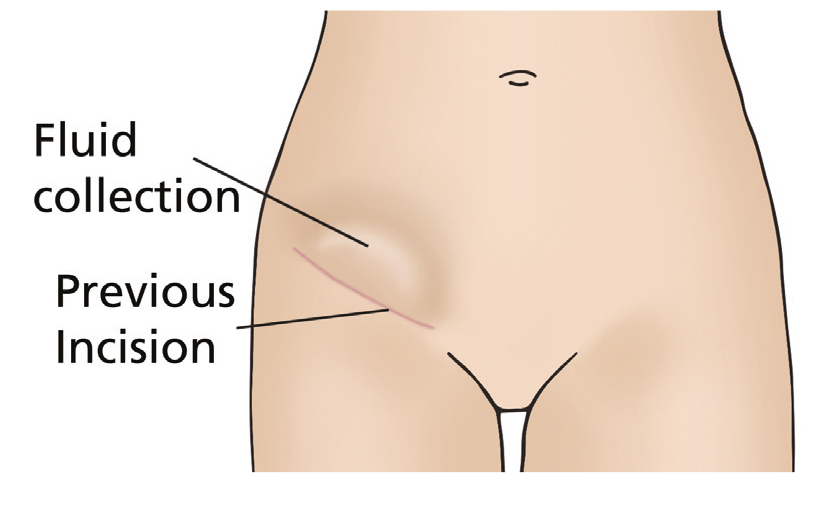
- Lymphocyst; this is a fluid collection at the site where lymph nodes have been removed. The fluid is often naturally reabsorbed by your body but may require draining if large or causing you discomfort.
- If groin lymph nodes are removed you may also feel numbness in your outer thigh area after surgery. This usually improves over time but may leave you with some permanent numbness at the tops of your legs.
- Scarring – scar tissue may narrow the entrance to your vagina and make it painful to have penetrative sex. You may be able to stretch your vaginal opening using dilators. You would be shown how to use these by your doctor or nurse.
- Difficulty reaching climax – some women who have had a vulvectomy have a reduction in sexual desire or pleasure and may also have problems reaching orgasm. This is most likely if you’ve had to have your clitoris removed.
- Numbness, tingling and pins and needles – these are caused by nerve damage during surgery. They will slowly get better in time, but may not disappear completely.
Will I have a scar?
Yes, although it will fade, the size of the scar will depend upon how much tissue has been removed. If only a small amount of skin is removed, the scar may be almost invisible. If the tumour is larger, then the appearance of the vulva will be different than before. If the lymph nodes in your groin have been removed, you can expect scars in this area but they are usually hardly visible when healed.
Is there anything I should do to prepare for the operation?
Make sure that all of your questions have been answered and that you fully understand what is going to happen. You are welcome to visit the ward and meet the staff before you are admitted to hospital – ask your specialist nurse or pre-assessment nurse to arrange this.
You should eat a balanced diet and if you feel well enough, take some gentle exercise before your operation, as this will help your recovery afterwards. Your GP, practice nurse or the doctors and nurses at the hospital will be able to give you further advice about this.
Before you come into hospital for your operation, try to organise things ready for when you come home. If you have a freezer, stock it with easy to prepare food. Arrange for relatives and friends to do your heavy work (such as changing your bedding, vacuuming and gardening) and to look after your children, or other dependants if necessary. Arrange for somebody to take you home from hospital when you are discharged. If you think you may have problems coping at home, you can discuss this with the nurses on the ward.
Vulval hygiene
Before your operation
It is important that the vulval area is scrupulously clean before you have your operation so we ask that you have a bath or shower on the morning of your surgery.
Vulval care after your operation
It is very important to keep your wound clean. We will provide you with a bottle of a brown antiseptic liquid. Have a bath twice a day putting 2 capfuls of the antiseptic in the water as you run your bath. After bathing pat your wound dry with a soft clean towel or use a hairdryer on a cool setting. If you do not have access to a bath or find it difficult to access one we suggest ordering a ‘sitz bath’. This is a plastic bowl that sits over the top of a toilet that you can fill with water (adding half a capful of the antiseptic liquid) and use to bathe the wound. These are available from websites such as Amazon and it is best to order prior to surgery. We will also provide you with a tube of specialist antiseptic gel to apply to your wound twice a day after bathing. The gel has anti-bacterial properties which can reduce your risk of infection whilst also supporting your wound to heal. Apply a pea size amount of gel to your wound twice a day until you have fully healed.
General advice after surgery
If you have had lymph nodes removed from one or both groins, you will have a tube called a drain coming out of each groin wound. This is to drain fluid that collects in the area and to help prevent swelling and infection. These drains can stay in for up to three weeks and you can go home with them still in. They are usually removed when you return for your out-patient clinic appointment. Initially the drainage tubes will be long and attached to a suction drain. Before you go home the tubes are cut down to just above your skin and a small bag is put over them which sticks to your skin. You will be shown how to measure the amount of fluid draining and empty the bags yourself. District nurses are usually arranged to support you with the drains at home.
At Home
- Take your painkillers regularly throughout the day to keep on top of any soreness or pain. You may find it sore to sit down for a few weeks.
- Try putting your feet up on your sofa or on a foot stool to take the pressure off your wound. You could try sitting on two cushions leaving a gap between them and positioning your wound over the gap.
- Take laxatives to make sure you don’t get constipated.
- If passing urine makes your wound sting, try pouring a small jug of warm water over your wound whilst you are sitting on the toilet.
- Avoid wearing tight clothing and do not use any lotions, perfumes and talcum powders in the area where you have had your operation.
- If you can avoid wearing underwear then this may keep you more comfortable. However, if you have bleeding from your wound you may need to wear underwear to keep a sanitary pad in place.
- Avoid washing underwear in biological washing powders – use non-biological instead.
- Please note that it is normal to experience a small amount of bleeding/loss until your wound has fully healed. This may take a number of weeks – sometimes months.
If you develop heavy bleeding, an offensive discharge or increasing pain then you should contact your GP as you may have an infection. If you experience tenderness, swelling, redness, warmth or pain in your lower leg then you should see your GP or visit the Accident and Emergency (A + E) department as soon as possible as you may have a blood clot in your leg (deep vein thrombosis). If you suddenly develop shortness of breath, chest pain or are coughing up blood then ring 999 as you could have a blood clot in your lung (pulmonary embolism) which is a medical emergency.
Is it normal to feel weepy or depressed after my operation?
Yes. It is a very common reaction to the operation. Most women feel shocked and upset by the idea of having surgery to the vulva. If these feelings persist when you leave the hospital, you may wish to discuss them with your GP or specialist nurse. There are also local and national support groups that you can contact. Details are given at the end of this booklet.
When can I have sex?
You may not feel physically or emotionally ready to start having sex again for a while. It can take several months for the vulval area to heal and for sensation to improve. If your clitoris has been removed as part of the surgery, your sexual response will feel different.
It can also take time for energy levels and sexual desire to improve. During this time, it may feel important for you and your partner to maintain intimacy, despite refraining from sexual intercourse. It can also be a worrying time for your partner. They should be encouraged to be involved in discussions about the operation and how it is likely to affect your relationship afterwards. Their involvement can have a positive influence on your recovery.
If you do not have a partner at the moment you may have concerns either now or in the future about starting a relationship after having this operation. Please discuss any concerns you have with your nurse specialist or consultant.
Will I need to visit the hospital again after my operation?
Yes. It is very important that you attend any further appointments arranged either at
St James’s Hospital, Bexley Wing, Leeds or at the local hospital that referred you for your treatment. The tissue results (histology) from your operation can take around 3 weeks.
An appointment for the outpatient clinic will be made to discuss these results with you and if any further treatment is necessary. If the cancer has not been fully removed or if cancer is found in your lymph nodes, you may be referred to a clinical oncologist for consideration of further treatment.
Additional information
Lymphoedema
This is a condition that can occur if you have lymph nodes removed during your surgery and is referred to earlier in this booklet as a risk of vulval surgery. By taking certain precautions you can try to prevent it occurring. There is a separate booklet, specifically about lymphoedema, that you can read but here are a few points:
- It is very important to keep your skin in good condition, as any injury or break in skin can cause infection which increases the risk of lymphoedema.
- Keep your skin well moisturised to keep it in good condition.
- Avoid extremes of heat and cold e.g. saunas, very hot baths/showers, ice packs.
- Avoid getting sunburnt. Wear high factor sunscreen and keep in the shade where possible.
- Use insect repellents to prevent insect bites.
- Avoid having injections to your legs.
- Take care to prevent scratches and cuts – if they do occur, wash them thoroughly and apply an antiseptic cream. If you notice any signs of redness or soreness of the skin, inform your GP.
- Use an electric razor or depilatory cream to remove unwanted hair on the legs. Do not use a razor blade.
- Take care when cutting your toenails – use nail clippers.
Useful Numbers
For queries regarding your admission please call the relevant secretary.
For advice on any medicines you have received from the hospital call:
Website
- To find our website go to https://www.leedsth.nhs.uk
- Click on services, then A-Z , Select G, then select Gynaecological cancer surgery
- Or alternatively type this; https://www.leedsth.nhs.uk/a-z-of-services/leeds-cancer-centre/your-treatment/surgery/gynaecological-surgery/
- On this website you will find information about our team, what we do, information leaflets and videos.
Contacts
- For advice please call your Clinical Nurse Specialist (CNS) or Ward J98
If your nurse specialist is not available then please leave a message on the answering machine and they will ring you back. Please note this may not always be the same day.
In an EMERGENCY please attend your nearest Accident and Emergency Department.
Local Support Services
Leeds Cancer Support
Leeds Cancer Support complements care provided by your clinical team. We offer access to information and a wide range of support, in a welcoming environment for you, your family and friends.
We can be found in the information lounges in Bexley Wing and also in the purpose built Sir Robert Ogden Macmillan Centre (behind the Thackray Medical Museum).
The Sir Robert Ogden Macmillan Centre
This centre offers a variety of free health & wellbeing and supportive therapies for patients, their family members and carers. These include hypnotherapy, mindfulness coaching, acupuncture (for hot flushes) and pilates.